Timing of Life-Sustaining Treatment Decisions Is Crucial
Early Planning Cuts End-of-Life Medical Expenses in Half
Last-Minute Choices Lead to Higher Costs and Intensive Care
If the decision to discontinue life-sustaining treatment is made one month before death, medical expenses during the final month are reduced by half. However, if the decision is made hastily just before death, medical costs actually increase significantly.
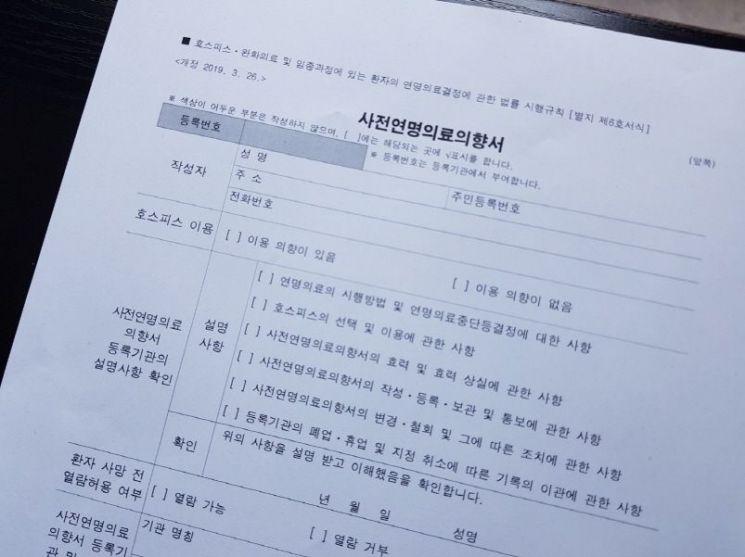 Advance Directive for Life-Sustaining Treatment. National Bioethics Policy Institute Life-Sustaining Treatment Management Center, Yonhap News
Advance Directive for Life-Sustaining Treatment. National Bioethics Policy Institute Life-Sustaining Treatment Management Center, Yonhap News
According to Yonhap News on August 12, the Health Insurance Research Institute under the National Health Insurance Service analyzed the impact of the timing of life-sustaining treatment discontinuation decisions on medical expenses in a report that precisely compared end-of-life medical costs between two groups: approximately 44,425 people who discontinued life-sustaining treatment and 44,425 general decedents, based on big data from about 350,000 deaths in 2023.
According to the report, patients who decided and implemented the discontinuation of life-sustaining treatment more than 30 days before death incurred an average of about 4.6 million won in medical expenses during their final month. This is only about half the average medical expenses (approximately 9.1 million won) incurred by general decedents without any advance planning during the same period.
The cost of direct life-sustaining treatments, such as cardiopulmonary resuscitation and mechanical ventilation, also dropped to about 500,000 won when the decision was made a month in advance, which is only a quarter of the 1.89 million won spent by general decedents.
Among those who discontinued life-sustaining treatment, about 73% made the decision less than a month before death. In particular, for the group that decided to discontinue between 8 and 30 days before death, medical expenses during the final month soared to 18 million won, nearly twice as much as those incurred by general decedents.
The research team explained, "This is because expensive medical procedures are concentrated right up until the discontinuation decision is made," adding that this demonstrates how crucial it is for discussions about discontinuation to take place in a timely manner.
The patient’s clear expression of intent also proved to be an important variable. When patients themselves decided to discontinue life-sustaining treatment, end-of-life medical expenses were lower than when the decision was made by family members. This suggests that the clearer the patient’s wishes, the more unnecessary treatments can be avoided in clinical settings, allowing for quicker decisions.
In addition, the life-sustaining treatment decision system was found to have positive ripple effects beyond the seven types of legally regulated life-sustaining treatments (such as cardiopulmonary resuscitation, hemodialysis, chemotherapy, and mechanical ventilation). The group that implemented discontinuation had lower rates of costly CT scans and high-nutrition intravenous infusions compared to the general decedent group, and while their intensive care unit utilization was lower, their hospice utilization was higher. This shows that the system can function as a comprehensive end-of-life care plan that helps patients experience a more comfortable final stage, rather than simply discontinuing treatment.
The report stated, "We confirmed that planning from a long-term perspective, rather than making decisions when death is imminent, results in lower pre-death medical expenses," and recommended, "Advance care planning should begin earlier so patients can make thoughtful decisions about their own care, and this should be supported by social discussions and institutional improvements."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.
![Clutching a Stolen Dior Bag, Saying "I Hate Being Poor but Real"... The Grotesque Con of a "Human Knockoff" [Slate]](https://cwcontent.asiae.co.kr/asiaresize/183/2026021902243444107_1771435474.jpg)














