Research has found that inflammation within the placenta can affect the fetal immune system and may be a cause of excessive allergic reactions in children after birth. This study is significant as it suggests new possibilities for the early prediction and prevention of allergic diseases such as pediatric asthma.
KAIST announced on August 4 that Professor Lee Heungkyu's research team from the Department of Biological Sciences has identified that inflammation occurring during pregnancy can influence the fetal stress response regulation system through the placenta. This, in turn, increases the survival and memory capabilities of T cells (key cells in the adaptive immune system), which can result in stronger allergic reactions in children after birth.
This finding was demonstrated through experiments on mice.
For the experiment, the research team induced inflammation in the placenta by injecting mice with lipopolysaccharide (LPS), a substance that triggers immune system inflammatory responses.
During this process, the placental tissue showed an increased level of a signaling molecule called tumor necrosis factor-alpha (TNF-α) due to the inflammatory response. This led to the activation of immune cells known as neutrophils, resulting in inflammatory damage to the placenta. Neutrophils are the most abundant type of white blood cell in the human body (comprising 40?75%), playing a key role in innate immunity and in eliminating invading bacteria and fungi.
The inflammatory damage to the placenta caused by increased neutrophil activity leads to stress in the fetus. In addition, the large secretion of stress hormones (glucocorticoids) induces significant changes in the fetal immune system. According to the research team, this causes fetal T cells to survive longer and enhances their memory function.
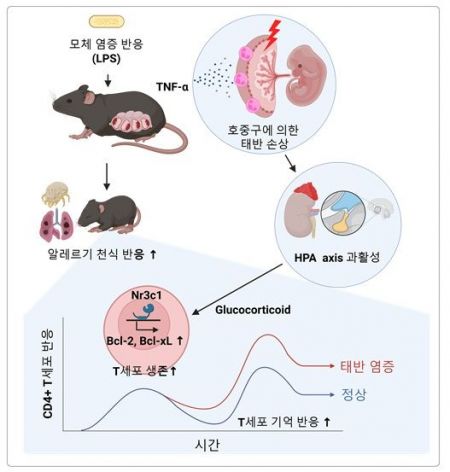 Schematic diagram of the mechanism by which maternal inflammatory response increases allergic immune response in children. Provided by KAIST
Schematic diagram of the mechanism by which maternal inflammatory response increases allergic immune response in children. Provided by KAIST
Notably, T cells formed through this process exhibited excessive allergic responses each time they were repeatedly exposed to antigens after birth. In fact, when the airways of the mice were exposed to house dust mite allergens, a strong eosinophilic inflammatory response and excessive immune activation were observed, with an increase in immune cells important for allergic and asthmatic reactions.
Professor Lee Heungkyu stated, "This study is the first in the world to identify how maternal inflammatory responses affect the fetal allergic immune system through the placenta," adding, "The results provide important scientific evidence for the development of biomarkers for early prediction and preventive strategies for pediatric allergic diseases in the future."
Meanwhile, Dr. Kwon Myungseung from the KAIST Graduate School of Medical Science (currently a clinical instructor in gynecologic oncology at Konyang University Hospital) participated as the first author of this study.
This research was conducted as part of the Individual Basic Research Program and the Bio-Medical Technology Development Program supported by the Ministry of Science and ICT and the National Research Foundation of Korea. The results (paper) were published on July 1 in the journal "Mucosal Immunology," which specializes in mucosal immunology.
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.
![Clutching a Stolen Dior Bag, Saying "I Hate Being Poor but Real"... The Grotesque Con of a "Human Knockoff" [Slate]](https://cwcontent.asiae.co.kr/asiaresize/183/2026021902243444107_1771435474.jpg)














