'Policy Forum on Non-Covered Service Management and Real-Expense Insurance Reform'
Unnecessary Mild and Non-Covered Items Converted to 'Managed Care'
Limit Coverage for Concurrent Treatments like Manual Therapy and Cosmetic Procedures
Encourage Transition to 5th Generation Real-Expense Insurance... Focus on Severe Cases
The government will designate certain non-severe and non-reimbursable treatments, such as manual therapy, as 'managed care,' requiring patients to bear more than 90% of the cost themselves. When unnecessary non-reimbursable and reimbursable treatments are performed simultaneously, health insurance benefits will be restricted. Additionally, for the 5th generation indemnity insurance, a plan focusing coverage on severe diseases will also be pursued.
On the 9th, the Ministry of Health and Welfare held a 'Policy Forum on Non-Reimbursable Care Management and Indemnity Insurance Reform' at the Korea Press Center and disclosed the policy direction centered on these contents. This improvement plan was formulated based on discussions from the Presidential Commission on Medical Reform.
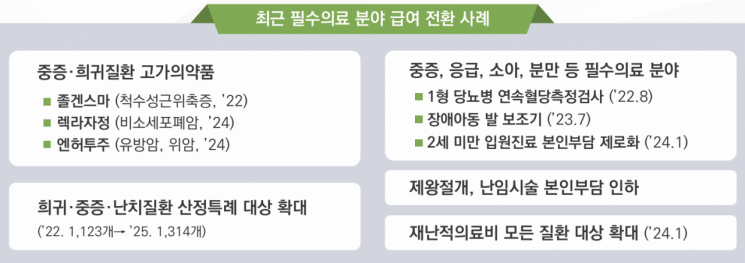
The government first decided to significantly strengthen management of non-reimbursable treatments, which are considered a major cause of rising medical expenses. They plan to convert non-reimbursable items with high risk of overuse into managed care, integrating them into the health insurance system and applying a patient co-payment rate of 90-95%. Once converted to managed care, prices and treatment standards can be set and managed within the health insurance system. This will unify the currently highly variable non-reimbursable treatment costs across medical institutions.
The managed care conversion will be prioritized for items where treatment volume suddenly increases or where there is excessive cost disparity among medical institutions, monitored through non-reimbursable reporting systems. Manual therapy, which has been the top non-reimbursable treatment cost, along with extracorporeal shock wave therapy and nutritional injections, are expected to be included first.
When performing non-reimbursable treatments such as cosmetic or plastic surgery while simultaneously claiming indemnity insurance for reimbursable treatments, the government will also implement 'parallel treatment reimbursement restrictions,' requiring patients to bear the reimbursable treatment costs as non-reimbursable. However, separate criteria will be established to recognize reimbursable treatments if medically necessary, ensuring no patients are disadvantaged by these restrictions. Furthermore, through re-evaluation of non-reimbursable items, the intended use and target will be clarified, and items lacking safety and efficacy after re-evaluation will be phased out.
The names of some non-reimbursable items, which vary by medical institution, will be standardized. Information such as prices of non-reimbursable items, total treatment costs, price differences by type of medical institution and region, safety and efficacy evaluation results, and alternative reimbursable items will also be disclosed. A plan will be established to strengthen patient choice by mandating consent forms after explaining prices, prescription reasons, and alternative treatments during non-reimbursable care.
The outline of the 5th generation indemnity insurance, which limits coverage for non-severe and non-reimbursable care and focuses on severe cases, has also emerged. A plan is underway to differentiate patient co-payment rates between general and severe patients in reimbursable treatments. For general patients, the co-payment rates for reimbursable treatments will be aligned with the health insurance co-payment rates and indemnity insurance co-payment rates, while for severe patients such as those with cancer, cerebrovascular and heart diseases, and rare diseases, a minimum co-payment rate of 20% will be applied to maintain the current coverage level.
For the upcoming 5th generation indemnity insurance, initially only severe non-reimbursable items will be covered, and after evaluating the management status of non-reimbursable items, products covering non-severe cases will be launched after June 2026. The review of non-reimbursable items with frequent indemnity claims will also be strengthened. The Financial Supervisory Service will verify whether medical acts were performed for treatment purposes in non-reimbursable cases where insurance payment disputes are frequent.
The government also plans to design the 5th generation indemnity insurance focusing on severe cases and promote a buy-back program that offers compensation to early subscribers of the 1st and 2nd generation indemnity insurance to encourage conversion, aiming for fundamental reform of indemnity insurance.
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.