Vertex and CRISPR Jointly Developed 'Casgeobi'
Approved by UK MHRA... FDA Approval Expected Next Month
Anemia Disease with No Treatment Other Than Bone Marrow Transplant
'Complete Cure' Effect with Gene-Edited Stem Cells
The world's first 'gene editing therapy' has been approved. An era has opened where diseases caused by genes can be edited to cure patients.
Vertex Pharmaceuticals and CRISPR Therapeutics announced on the 16th (local time) that the UK Medicines and Healthcare products Regulatory Agency (MHRA) has conditionally approved the gene editing therapy 'Casgevy' for the treatment of sickle cell disease (SCD) and transfusion-dependent beta-thalassemia (TDT). The company expects that about 2,000 patients in the UK will be able to receive treatment with Casgevy.
With this, Casgevy has become the world's first approved gene editing therapy. Developed under the name 'Exa-Cell,' the therapy is also undergoing approval review by the U.S. Food and Drug Administration (FDA) for the SCD indication, with a deadline of July 8 next month. Reshma Kewalramani, CEO of Vertex, emphasized, "Today is a historic day in medical science," adding, "The approval of Casgevy is the world's first approval of a CRISPR-based therapy."
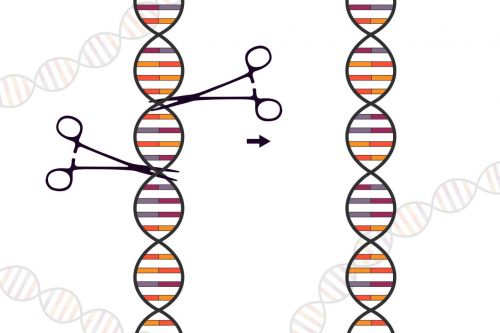
Casgevy is a 'one-shot' therapy that can cure the disease with a single administration. The problematic gene is edited using 'CRISPR-Cas9' technology in stem cells extracted from the patient, which are then reintroduced into the patient. These stem cells engraft in the bone marrow and reconstruct the patient's immune system. In fact, patients participating in clinical trials have maintained the drug's efficacy for up to three years after administration.
SCD is a fatal disease where red blood cells, which should be round, become sickle-shaped, impairing oxygen transport, with an average patient death age of 40. TDT is also a disease caused by problems with beta-globin in hemoglobin within red blood cells, with no cure other than stem cell donation, and patients typically die at an average age of 55. Both diseases had no cure other than bone marrow (hematopoietic stem cell) transplantation, but now treatment with drugs is possible.
Casgevy is expected to become the most expensive drug in the world upon release. The market currently estimates the launch price of Casgevy to be between $4 million and $6 million (approximately 5.2 billion to 7.8 billion KRW). This far exceeds the previous world's most expensive drug, CSL Behring's hemophilia B treatment 'Hemgenix,' priced at $3.5 million (about 4.5 billion KRW).
This approval is the result of 12 years since discussions on gene scissors technology began in earnest. Although there were first- and second-generation technologies earlier, the development of the third-generation CRISPR-Cas9 technology in 2011 opened the way for full-scale development. Professor Emmanuelle Charpentier of the Max Planck Institute first announced its existence, and through joint research with Professor Jennifer Doudna of UC Berkeley, they succeeded in reproducing gene scissors in vitro. The two jointly received the 2020 Nobel Prize in Chemistry.
With the emergence of the first gene editing therapy, the related market is expected to grow rapidly. The Korea Research Institute of Bioscience and Biotechnology forecasts that the global gene editing market will grow from $5 billion (about 6.5 trillion KRW) this year at an average annual rate of about 15%, doubling to $10 billion (about 13 trillion KRW) by 2028.
Overseas, companies such as Vertex, CRISPR, and Verve Therapeutics are growing rapidly, and in June, Eli Lilly licensed cardiovascular therapies developed by Verve for up to $600 million, showing increasing interest from big pharma. In Korea, ToolGen, founded by former Seoul National University professor Jin-Soo Kim, who succeeded in the world's first human gene editing using gene scissors in 2013, is developing treatments such as 'TGT-001' for the rare disease Charcot-Marie-Tooth disease (CMT).
However, safety concerns remain an obstacle. The FDA advisory committee has recommended that even if Exa-Cell is marketed, patients' conditions should be monitored for about 15 years. While the efficacy of Exa-Cell is clear given the lack of previous treatments for these diseases, this recommendation reflects concerns that gene editing technology may cause unintended genetic changes.
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.