 Atopic dermatitis. [Image source=Irasutoya.com]
Atopic dermatitis. [Image source=Irasutoya.com]
Atopic dermatitis is a common allergic disease that is difficult to treat. For this reason, it is considered one of the clear 'main enemies' by parents raising children. The main symptoms include severe itching, extreme sensitivity to external stimuli or allergy-inducing substances, and eczema-like changes caused by scratching the skin. Moreover, it chronically recurs, and although it tends to decrease with age, it repeatedly worsens and improves from childhood through adolescence to adulthood. The incidence has been steadily increasing; according to the National Health Insurance Review and Assessment Service's statistics on diseases of public interest, the number of atopic dermatitis patients rose from 920,000 in 2018 to 990,000 in 2021.
Although atopic dermatitis remains difficult to treat, ongoing research and new drug development are gradually opening the path to conquering it. Recently, notable related studies have continued in the medical field. Researchers have succeeded in developing methods to predict the onset before symptoms appear and have identified substances that could aid new drug development. Research on oral immunotherapy using probiotics has also shown promising results, indicating remarkable progress in various areas.
 Professor Ahn Gang-mo (left) and Professor Kim Ji-hyun, Department of Pediatrics and Adolescents, Samsung Medical Center.
Professor Ahn Gang-mo (left) and Professor Kim Ji-hyun, Department of Pediatrics and Adolescents, Samsung Medical Center. [Photo by Samsung Medical Center]
Recently, a globally notable study was published by Korean and American researchers. They succeeded in identifying lipid biomarkers in the skin that can predict the risk of developing atopic dermatitis. The joint research team, including Professors Kangmo Ahn and Jihyun Kim from the Department of Pediatrics at Samsung Medical Center, and Professors Donald Leung and Yevgeniy Berdyshev from National Jewish Health in the United States, collected stratum corneum samples from the arms of 111 two-month-old infants without skin abnormalities using tape stripping, analyzed skin lipid composition and cytokines, and followed up until 24 months of age.
Through this, the team confirmed that changes in skin lipid composition and cytokines occur as early as two months of age, before the onset of atopic dermatitis. In particular, infants with a family history of allergies who had high levels of IL-13 protein and 26:1 unsaturated sphingomyelin in the skin, and low levels of protein-bound ceramide (O30:0(C20S)-CER), showed up to a 54-fold increased risk of developing atopic dermatitis. This study was published in the Journal of Allergy and Clinical Immunology (IF=14.29) and was introduced at the American Academy of Allergy, Asthma & Immunology conference held in the United States at the end of last month, attracting attention. The research team explained, "Predicting the onset of atopic dermatitis is very important as early intervention can reduce patients' suffering and decrease medical burdens," adding, "It is expected to prevent disease progression leading to the allergic march and open the foundation for personalized treatment considering individual characteristics in the future."
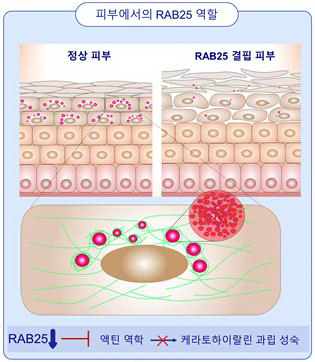 It was confirmed that when RAB25 is deficient, cell motility decreases, leading to inhibited growth of keratohyalin granules. This had a negative impact on skin hydration and other factors.
It was confirmed that when RAB25 is deficient, cell motility decreases, leading to inhibited growth of keratohyalin granules. This had a negative impact on skin hydration and other factors. [Photo by Yonsei Medical Center]
Research to advance treatments and therapies for atopic dermatitis is also actively underway. A research team led by Professors Kitaek Nam from the Department of Biomedical Sciences and Changwook Park from the Department of Dermatology at Yonsei University College of Medicine reported that a deficiency of the 'RAB25' protein inhibits the production of keratohyalin granules involved in skin moisture retention, reducing the moisturizing factor called 'filaggrin' and worsening atopic dermatitis. Comparing and analyzing protein expression levels in normal skin and atopic dermatitis skin cells, they found that RAB25 protein expression in atopic dermatitis was only 1/36th of that in normal skin samples. Furthermore, animal experiments confirmed that injecting calpeptin, which restores skin cells, into RAB25 protein improved atopic dermatitis symptoms.
Efforts to enhance the treatment effects of atopic dermatitis and allergies with the help of probiotics are also gradually gaining ground. According to Professor Kangmo Ahn's research, after taking kimchi-derived probiotics, the atopic dermatitis severity index (SCORAD) decreased from 29.5 points to 16.4 points after 12 weeks of intake, a reduction of about 44%. This index uses 25 points as the threshold to distinguish severity, and a score in the 16-point range is considered mild. In a paper published by Professor Jihyun Kim in August last year, it was also demonstrated that Bifidobacterium longum (Bifidus bacteria), a type of probiotic, effectively alleviates skin barrier dysfunction and improves atopic dermatitis. Professor Kim stated, "Oral immunotherapy using probiotics is a newly emerging field," adding, "We will continue to strive in research so that patients can be free from atopic dermatitis as well as food allergies."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.
![Clutching a Stolen Dior Bag, Saying "I Hate Being Poor but Real"... The Grotesque Con of a "Human Knockoff" [Slate]](https://cwcontent.asiae.co.kr/asiaresize/183/2026021902243444107_1771435474.jpg)














