NHIS Blocks 10.8 Billion Won in Long-Term Care Fund Leakage
The National Health Insurance Service announced on December 17 that it has decided to award a total of 660 million won in rewards to 142 individuals who reported long-term care institutions for fraudulent claims this year.
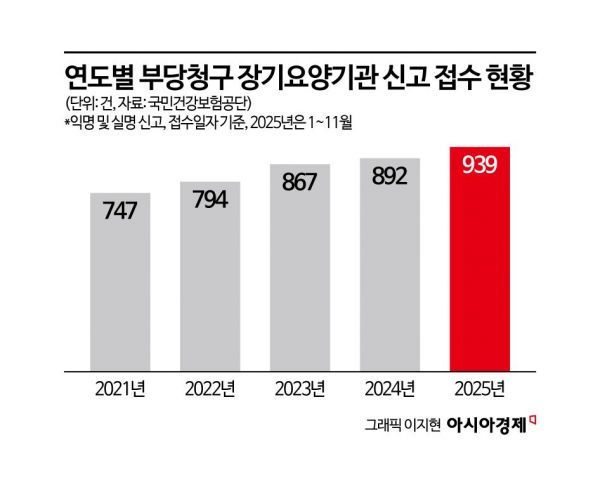
From January to November this year, there were a total of 939 cases of fraudulent claims by long-term care institutions reported by internal staff and users. Of these, 142 reports were approved for reward payments, amounting to a total of 10.859 billion won. The highest single reward paid was 62 million won.
In one case, the head of a long-term care institution, identified as Mr. A, violated the full-time employment requirement for 33 months by engaging in club activities during work hours. He falsely registered work hours and fabricated records to make it appear as if he had provided services such as home bathing to beneficiaries, submitting over 3,000 fraudulent claims for service fees.
In another case, the head of a different institution, identified as Mr. B, intentionally underreported the number of staff members to falsely receive additional personnel support payments, and falsely registered the working hours of an affiliated cook for 25 months to claim salary payments.
The "Reward System for Reporting Fraudulent Claims by Long-Term Care Institutions" has been in operation since 2009 to strengthen monitoring through public participation and prevent financial leakage. If a person related to a long-term care institution files a report, the maximum reward is 200 million won, while users of the institution or other reporters can receive up to 5 million won.
Reports of fraudulent claims by long-term care institutions can be submitted via the Long-Term Care Insurance for the Elderly website, The Health Insurance (mobile app), by mail, or directly to the Service.
Kim Gihyung, Executive Director of Long-Term Care at the National Health Insurance Service, stated, "The long-term care insurance system is operated with premiums paid by the public, so public interest and participation are the most powerful drivers in preventing fraudulent claims. We will actively operate the reward system for reporting to create an environment where honest long-term care institutions are fairly evaluated and to establish a foundation where beneficiaries can use services with peace of mind."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.
![Clutching a Stolen Dior Bag, Saying "I Hate Being Poor but Real"... The Grotesque Con of a "Human Knockoff" [Slate]](https://cwcontent.asiae.co.kr/asiaresize/183/2026021902243444107_1771435474.jpg)










