Health Insurance Policy Committee Establishes 487 New Surcharge Items for Surgeries on Patients Aged 6 to 15
Compensation for Early Cervical Conization Strengthened
Digital Tomosynthesis for Breast Cancer Now Covered by Insurance
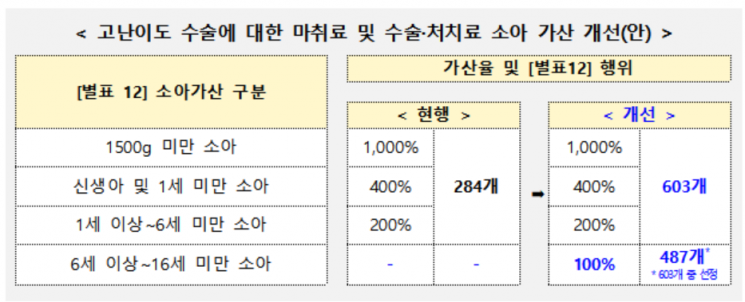
The number of health insurance surcharge items for anesthesia fees and others in high-difficulty pediatric surgeries will be significantly increased. For surgeries on children and adolescents aged 6 and above but under 16, new surcharge items that did not exist before will be established and surcharged at 100%.
On the 27th, the Ministry of Health and Welfare announced that it held the '4th Health Insurance Policy Deliberation Committee (HIPS) in 2025' and approved agenda items including strengthening compensation for high-difficulty pediatric surgeries and enhancing coverage for gynecologic cancer treatment.
Pediatric surgeries differ from adult surgeries in that they must consider characteristics according to growth and developmental stages, making them fields with higher difficulty, risk, and resource consumption, thus the need for additional compensation has been continuously raised.
Accordingly, the Ministry of Health and Welfare has continuously communicated with pediatric surgical societies and comprehensively considered resource input such as pediatric-customized equipment and specialized personnel, difficulty, risk, and disease characteristics. As a result, it decided to add 319 items to the existing 284 high-difficulty pediatric surgery fee schedule items for children under 6, totaling 603 items to be surcharged.
Additionally, considering the growth and developmental period requiring high-difficulty surgery, the target age range will be expanded to 6 years and above but under 16 years, establishing 487 new surcharge items and improving the fee schedule criteria to reflect disease characteristics requiring staged surgeries in 15 surgical procedures.
The Ministry stated, "Considering the urgency and importance of maintaining pediatric surgical infrastructure, we prioritized adding and strengthening compensation for high-difficulty surgery items reflecting the growth and developmental characteristics of children. Going forward, we plan to sequentially strengthen compensation for surgeries that are highly difficult and resource-intensive but relatively undervalued."
Health insurance compensation for gynecologic cancers such as cervical cancer and breast cancer will also be strengthened. These cancers require early and active treatment due to increasing incidence, advances in diagnostic methods, and the importance of prognosis after surgery, with high demand from patients and medical fields.
The HIPS decided to strengthen compensation levels for cervical conization and convert non-covered breast cancer digital tomosynthesis to covered services. When young women contract cervical cancer, fertility can be preserved through cervical conization rather than extensive hysterectomy. However, until now, there was no procedure classification, and a low fee was applied. Going forward, compensation will be increased to 121% of the standard previously applied under 'extensive hysterectomy and bilateral pelvic lymphadenectomy.'
The only treatment approved domestically for the rare disease 'transthyretin amyloid cardiomyopathy,' Vyndamax capsules, will also be covered by health insurance starting next month. Vyndamax capsules are the only treatment approved by the Ministry of Food and Drug Safety for transthyretin amyloid cardiomyopathy, stabilizing transthyretin to inhibit amyloid formation and clinically proven to reduce cardiovascular hospitalization rates and mortality. This disease is especially subject to a rare disease special case with a 10% patient co-payment rate, so the patient's annual drug cost burden, which previously reached 36.5 million KRW, is expected to be significantly reduced to about 3.65 million KRW.
A Ministry of Health and Welfare official said, "We are continuously strengthening coverage by listing new drugs essential for patients such as those for severe and rare diseases, leukemia, and anticancer drugs, and expanding the usage scope of existing drugs. We hope that through the health insurance coverage of this treatment, patients and their families will reduce their economic burden for treatment, recover their health, and return to daily life."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.