National Health Insurance Service, 11.4 Billion KRW in Improper Claims This Year
Strengthening Oversight of Fraudulent Activities Through Enhanced Whistleblowing
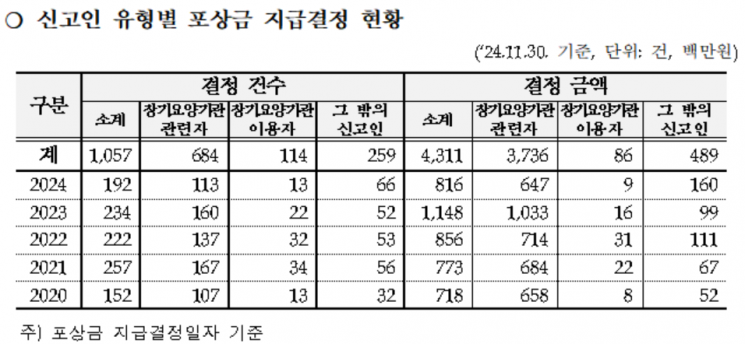
The National Health Insurance Service announced on the 11th that it has decided to pay a total of KRW 816 million in rewards to 192 people who reported long-term care institutions that fraudulently claimed a total of KRW 11.441 billion in long-term care benefits this year, with a maximum of KRW 47 million per person.
The Service has been paying a portion of the collected amount as rewards to those who report fraudulent long-term care institutions since 2009 to promote a healthy culture of long-term care benefit claims and prevent financial leakage.
Accordingly, from 2020 to November of this year, 3,647 reports of fraudulent acts were received, and KRW 4.311 billion in rewards were decided for 1,057 cases where the reported facts were confirmed.
Anyone, including employees or users who are aware of false or fraudulent acts by long-term care institutions related to long-term care benefit claims, can report. The reward can be up to KRW 200 million.
Reports of fraudulent claims can be made through the Elderly Long-Term Care Insurance website or the mobile application 'The Geongangboheom (The Health Insurance)', and are also possible via mail or by visiting the Service in person. Related consultations are available by calling the dedicated reporting consultation number.
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.