Financial Supervisory Service Publishes Cases of Insurance Payments for New Medical Technologies
Need to Check Ministry of Health and Welfare Notices to Determine Coverage for Actual Expense Insurance
Mr. A was diagnosed by his primary doctor as having no treatment options other than knee replacement surgery due to severe knee pain. Afraid of surgery, he delayed the procedure but later received knee stem cell injection treatment at another hospital after hearing about a new treatment method. He then filed an insurance claim, but it was denied. According to the Ministry of Health and Welfare’s notice, knee injections are only applicable for Kellgren-Lawrence (KL) grades 2 to 3 based on X-ray examination, but Mr. A’s grade was 4.
The Financial Supervisory Service disclosed on the 20th cases where insurance claims were denied after receiving expensive new medical technology treatments.
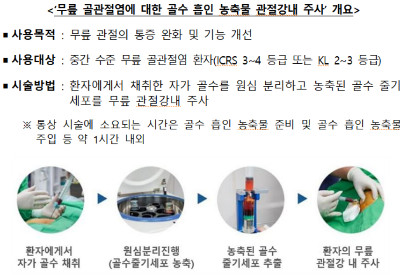
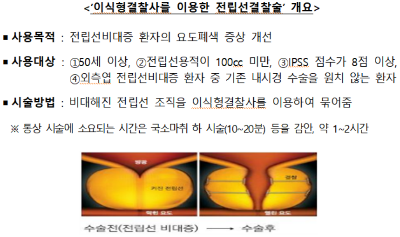
Recently, insurance claims and disputes regarding ‘bone marrow aspirate knee injections (knee stem cell injections)’ and ‘prostate embolization,’ which have been approved as new medical technologies by the Ministry of Health and Welfare notice, have been rapidly increasing for knee osteoarthritis. The insurance claim amount per knee stem cell injection ranges from 1 million to 26 million KRW. For prostate embolization, the amount varies greatly by hospital, ranging from 200,000 to 12 million KRW.
New medical technologies are covered by indemnity insurance, but if the treatment does not meet the criteria set by the Ministry of Health and Welfare notice, compensation may be denied. Before receiving new medical technology treatments such as knee stem cell injections or prostate embolization, it is essential to confirm through a doctor or insurance company whether the treatment meets the ‘treatment criteria’ specified in the Ministry of Health and Welfare notice. For knee stem cell injections, only 3rd and 4th generation indemnity insurance policies subscribed to after April 2017 provide coverage if a separate rider is purchased. Before treatment, policyholders must verify their indemnity insurance ‘subscription date and coverage’ with their insurance company.
Mr. B, in his 40s, was a patient with benign prostatic hyperplasia (BPH) who was undergoing medication treatment. He received the procedure upon recommendation from an acquaintance and filed an insurance claim, but it was denied because he did not meet the age criterion of 50 years or older, thus falling outside the treatment scope. Mr. C, who suffered from frequent urination and residual urine symptoms, underwent the procedure and filed an insurance claim, but it was denied. His prostate volume was 150cc, exceeding the notice’s standard, and there was a dispute over the diagnosis of BPH. A third medical opinion from a tertiary hospital concluded that the diagnosis was not recognized.
Prostate embolization is a treatment method for BPH patients who meet the following criteria: age 50 or older, prostate volume less than 100cc, International Prostate Symptom Score (IPSS) of 8 or higher, and lateral lobe prostate enlargement, and who do not want conventional endoscopic surgery. If any of these criteria are not met, insurance claims will be denied.
An official from the Financial Supervisory Service stated, "Many patients are misled by offers of free manual therapy or treatment discounts and rely solely on doctors’ assurances that indemnity insurance will cover expensive new medical technology treatments, only to find out later that their insurance claims are denied. Therefore, special caution is required."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.