Obesity, often cited as the root cause of many diseases, has once again been shown to aid treatment in cancer patients, revealing the so-called "obesity paradox." A study conducted by Korean medical professionals on colorectal cancer patients confirmed that a higher body mass index (BMI) is associated with better treatment outcomes. Notably, this study found that when both muscle mass and BMI increase together, the risk of death can be reduced, highlighting the importance for cancer patients to maintain weight and increase muscle mass.
Professors An Jung-bae and Kim Han-sang from the Department of Oncology at Yonsei Cancer Center, Professor Park Yu-rang from the Department of Biomedical Systems Informatics at Yonsei University College of Medicine, and intern researcher Seo Dong-jin from Severance Hospital recently published their findings in the international journal JMIR Public Health and Surveillance (IF 14.557). Their study showed that improving lifestyle habits such as exercise after a colorectal cancer diagnosis to increase muscle mass and BMI can reduce the risk of death by 32%. This is the first study to analyze cancer patient prognosis by simultaneously considering both obesity and muscle mass variables.
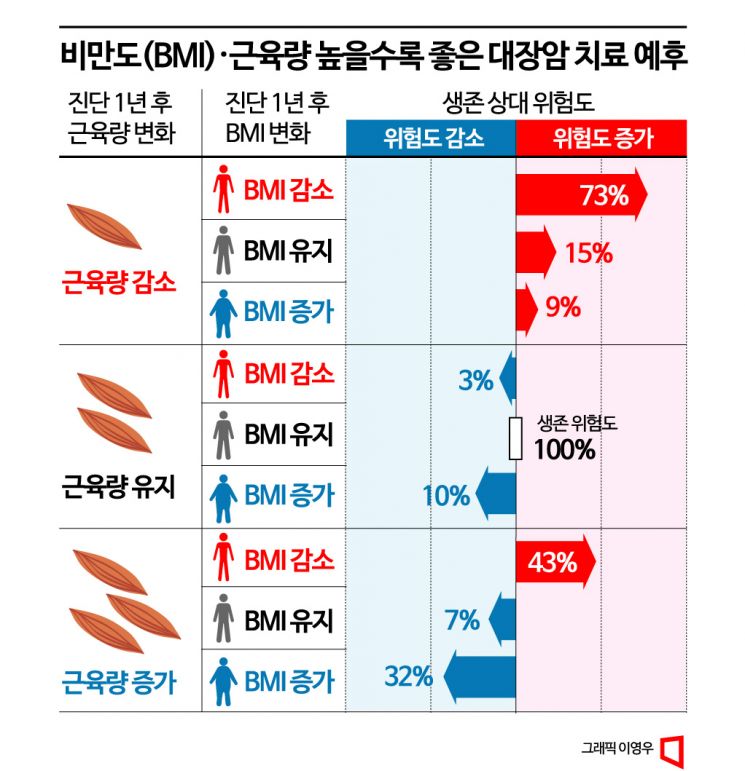
The research team analyzed 4,056 colorectal cancer patients treated at Severance Hospital between 2010 and 2020, examining how changes in BMI and muscle mass at diagnosis and at 1, 3, and 6 years post-diagnosis affected patient prognosis. Using the group with stable BMI and muscle mass (relative survival hazard ratio 1) as a baseline, they found that patients with increases in both BMI and muscle mass had a 32% lower relative risk of death (0.68). Conversely, patients with decreases in both variables had a 73% higher risk of death (1.73).
In particular, even in groups where muscle mass increased but obesity decreased, the relative risk of death was 43% higher (1.43) compared to the baseline, and in groups where muscle mass decreased but obesity increased, the relative risk was 9% higher (1.09). In other words, both weight and muscle mass need to increase to reduce the risk of death. Professor An Jung-bae explained, "For cancer patients, it is more important to gain weight rather than lose it, and maintaining muscle mass through health management can extend life expectancy." He added, "It is expected that not only chemotherapy but also exercise therapy and improvements in healthy lifestyle habits can increase the life expectancy of cancer patients."
The importance of weight management in cancer patient prognosis has been demonstrated in various studies. A study published last year by a research team at Samsung Seoul Hospital in the international journal PLOS ONE also found that obese patients had a lower risk of death after cancer surgery compared to patients with normal or low body weight. Obese patients (BMI 25 or higher) had a 31% lower risk of death than normal-weight patients (BMI 18.5 to less than 25) and a 62% lower risk than underweight patients (BMI less than 18.5). Notably, among obese patients, those with a BMI of 30 or higher had a 43% lower risk of death compared to normal-weight patients.
However, the "obesity paradox" is known to vary depending on cancer type and patient gender. Particularly, female cancers such as breast and gynecological cancers, which are closely linked to hormones affected by obesity, do not exhibit this paradox. Nevertheless, in cancer surgeries that impose significant physical burdens, being obese rather than underweight can facilitate relatively easier recovery of strength and provide the stamina needed to endure difficult treatment processes. Therefore, it is meaningful that cancer patients should improve their lifestyle habits by maintaining or increasing weight and increasing muscle mass.
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.