Death toll reaches record high of 216 on the past 5 days... 1,013 in the first week of March
Severe patients increasing, with more critical cases uncounted in statistics
Top-tier hospitals at breaking point... Actual bed occupancy rate in the Seoul metropolitan area exceeds 90%
 On the 6th, amid a large-scale COVID-19 outbreak causing an increase in pediatric cases, a staff member at a pharmacy in Seoul is displaying pediatric home treatment kits including fever reducers and cold medicine for children.
On the 6th, amid a large-scale COVID-19 outbreak causing an increase in pediatric cases, a staff member at a pharmacy in Seoul is displaying pediatric home treatment kits including fever reducers and cold medicine for children. [Image source=Yonhap News]
As the Omicron variant virus spreads explosively, the number of critically ill patients who have difficulty breathing on their own and are on ventilators or extracorporeal membrane oxygenation (ECMO) devices has approached 1,000. Over the past week, the number of deaths from COVID-19 has exceeded 1,000. There are also projections that once the pandemic passes its peak, the daily death toll could be two to three times higher than it is now.
Weekly Death Toll Exceeds 1,000
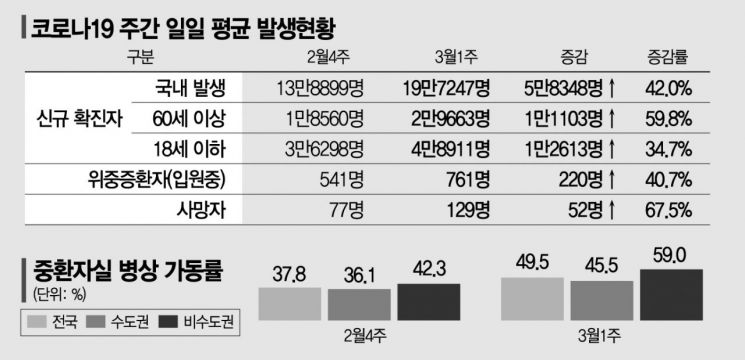
According to the Central Disease Control Headquarters on the 7th, the number of COVID-19 deaths announced on the 5th was 216, marking a record high, and 161 deaths occurred on the 6th. In the first week of March (February 28 to March 5), a total of 1,013 deaths were reported. Compared to the previous week (February 21?27), which had 539 deaths, this is nearly double the number.
The trend of critically ill patients, which is directly linked to the number of deaths, is also precarious. Over the past week, the number of critically ill patients has steadily increased from 715 (February 28) to 727, 762, 766, 797, 896, and 885. As of midnight on that day, the number of new confirmed cases increased by 210,716 (210,628 domestic cases) compared to the previous day, bringing the total confirmed cases to 4,666,977. The number of critically ill patients was 955, and the death toll was 139.
The number of severe patients not captured in statistics is also rising. Currently, out of 2,747 dedicated treatment beds for critically ill patients nationwide, 1,643 (59.8% occupancy rate) are in use. The remaining patients, excluding the 955 COVID-19 critically ill patients announced by the government, are COVID-19 confirmed patients whose underlying conditions have worsened and require intensive care. Moreover, while the occupancy rate of critical care beds in the metropolitan area is 55.9%, it has risen to 69.1% in non-metropolitan areas, indicating that the capacity to manage critically ill patients may soon reach its limit.
Experts predict that the aftermath will be more severe, considering that generally, deaths and critically ill patients begin to increase two to three weeks after new confirmed cases rise, and since the number of confirmed cases has not yet peaked. They also hold a pessimistic view regarding the quarantine authorities' claim that they can handle 2,200 to 2,500 critically ill patients.
Professor Eom Jung-sik of Gachon University Gil Medical Center's Department of Infectious Diseases questioned, "Out of about 2,700 critical care beds, about 1,200 remain, but how many of these are actually usable?" Professor Kim Tak of Soonchunhyang University Bucheon Hospital's Department of Infectious Diseases said, "It seems that all critical care beds in tertiary or university hospitals have already been exhausted. I hope the remaining critical care beds can perform well, but it does not look that hopeful. I think the time to selectively use critical care beds, as during the Delta wave, has already come."
The Medical Field Is Already in 'Panic'
Tertiary general hospitals treating critically ill COVID-19 patients have already reached a critical point. With up to 50 confirmed cases per day in some hospitals, medical gaps have become a reality. Regardless of the overall ICU bed occupancy rate, the occupancy rate of tertiary general hospitals in the metropolitan area that actually admit critically ill patients exceeds 90%, according to frontline medical staff. Problems such as patient waiting can occur when the critical care bed occupancy rate exceeds 80%, and differences in bed availability by region must also be considered.
Currently, Seoul National University Hospital and Asan Medical Center, among others, treat confirmed patients who are asymptomatic or have mild symptoms in general wards such as single rooms rather than isolation wards, even if confirmed cases occur in the ward. Previously, patients were moved to isolation wards within the hospital, but as the number of critically ill patients rapidly increased, it became difficult to allocate beds internally. Many tertiary general hospitals have also shortened the isolation period for confirmed medical staff from 7 days to 5 days according to the Business Continuity Plan (BCP) guidelines.
Since the phased return to normal life (With COVID) in December last year, the discharge order, which was implemented as critically ill patients rapidly increased, is now being reissued. The discharge order is a measure to move patients who have been treated in intensive care units for a certain period to other hospitals or wards to secure beds, a desperate measure by the quarantine authorities. However, concerns have been raised that patients such as cancer patients or transplant recipients with weakened immunity, who have not yet completed treatment or continue to shed the virus, could be moved to general wards simply because they are not receiving high-flow oxygen therapy.
Yeom Ho-gi, Chair of the COVID-19 Countermeasures Expert Committee of the Korean Medical Association, said, "Only the number of beds has increased, but the medical workforce remains the same, and medical staff working in intensive care units are already beyond burnout. Early detection and treatment of patients progressing to severe illness is most important."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.
![Clutching a Stolen Dior Bag, Saying "I Hate Being Poor but Real"... The Grotesque Con of a "Human Knockoff" [Slate]](https://cwcontent.asiae.co.kr/asiaresize/183/2026021902243444107_1771435474.jpg)










