Research Team Led by Professor Jang Young-tae at IBS
Identifies Fluorescent Substance That Shines Only in Antibody-Producing B Cells
Enables Isolation While Alive
Increases Potential for Applications Such as Disease Treatment Antibody Production
[Asia Economy Reporter Kim Bong-su] A technology has been developed that can distinguish B cells, which produce antibodies in the blood, in a 'living' state. This has attracted attention as it opens up possibilities for applications such as producing antibodies needed for treating various diseases.
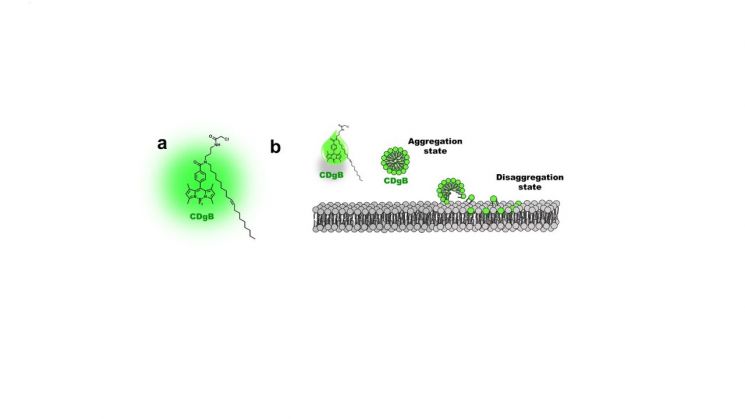
The Institute for Basic Science (IBS) announced on the 19th that the research team led by Deputy Director Jang Young-tae (Professor of Chemistry at POSTECH) of the Complex Systems Self-Assembly Research Center developed a new fluorescent molecule, ‘CDgB’, that can identify living B cells using only the characteristics of cell membrane lipids.
B cells exist in lymphocytes, which account for 25% of white blood cells. Along with T cells and NK cells, they are responsible for immunity. Unlike T cells and NK cells that kill viruses or cancer cells invading the body, B cells function to produce antibodies.
However, until now, there has been no method to distinguish B cells while they are alive. Previously, B cells were identified through the binding of the cell’s intrinsic biomarkers and antibodies, but this process caused the B cells to die.
The research team conceived the idea of identifying cells by using differences inherent to the cells themselves rather than conventional biomarkers such as proteins or carbohydrates. After isolating B cells and T cells from the spleen of a mouse, they injected 10,000 fluorescent molecules. Among them, they discovered a fluorescent molecule that selectively stains only B cells on the cell membrane and named it CDgB.
Senior Researcher Kwon Hwa-young of the team explained, “Hydrophobic CDgB forms nano-aggregates smaller than 100 nm in aqueous media similar to the body. These nano-aggregates do not fluoresce, but when they fuse with the cell membrane and bind to B cells, fluorescence is activated.”
The team predicted that CDgB would distinguish B cells from T cells based on differences in the length of cell membrane lipids and experimentally proved this. The cell membrane of B cells is relatively shorter in lipid length and contains less cholesterol, making it more flexible than that of T cells. When CDgB was applied to bone marrow cells, it was confirmed that the fluorescence intensity varied according to the flexibility of the cell membrane. CDgB emitted strong fluorescence in early-stage B cells with soft membranes but weak fluorescence in mature B cells with relatively less flexible membranes. In short, CDgB was confirmed as a tool that identifies cells based on fluorescence intensity and tracks changes in the cell membrane.
The researchers also improved CDgB to clearly distinguish B cells through stronger fluorescence. CDgB has a ‘carbon tail’ consisting of long chains of carbon atoms, and the fluorescence intensity varies depending on the length of this tail. Analysis showed that CDgB analogs with 16 to 18 carbon atoms connected exhibited high B cell selectivity.
Deputy Director Jang Young-tae said, “This research developed a new tool that can identify cells in a living state, replacing antibody-based identification technology. In the future, CDgB could develop into a tool that detects abnormalities in cells and predicts diseases early based on fluorescence intensity.”
The research results were published online on the 9th in the Journal of the American Chemical Society (JACS, IF 14.612), a prestigious journal in the field of chemistry.
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.