Choi Jong-yoon "Illegal Medical Institutions' Fraudulent Claims Total 2.6 Trillion Won Over 5 Years"
Recovery Amount per Institution Soars from 1.9 Billion to 8.7 Billion Won
'Granting Special Investigation Authority to NHIS' Failed to Pass in Last National Assembly
[Asia Economy Reporter Choi Dae-yeol] The scale of illegal medical institutions such as office-head hospitals is growing, but the amount recovered after detection is actually decreasing. An office-head hospital operates a medical institution by borrowing the name of a doctor or corporation from someone who is not authorized to open a medical institution, which leads to a decline in medical quality and the possibility of excessive treatment. It is also cited as a factor causing leakage in the National Health Insurance finances due to fraudulent billing of medical fees.
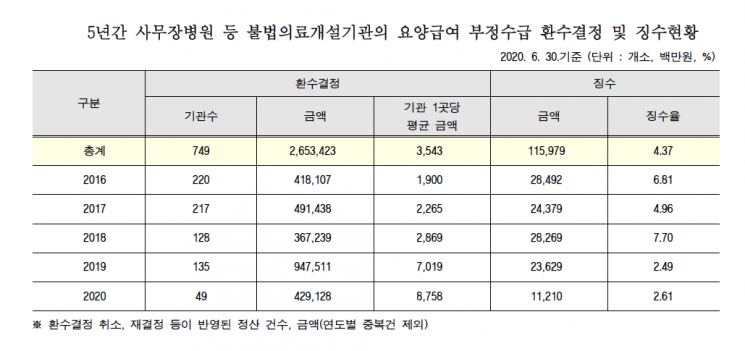
According to data on the status of recovery decisions and collections for fraudulent claims of medical benefits at illegal medical institutions, submitted by the National Health Insurance Service and disclosed on the 29th by Choi Jong-yoon, a member of the Democratic Party of Korea, the amount confirmed for recovery over the past five years totaled 2.6534 trillion won. Although the government’s eradication measures seemed to slow the trend in 2018, the amount immediately increased the following year. In 2018, 128 illegal medical institutions were subject to recovery decisions, amounting to 367.2 billion won, which was about 90 fewer institutions and approximately 25% less in amount compared to 2017.
However, in 2019, the number of institutions subject to recovery decisions rose to 135, with the amount increasing to 947.5 billion won. This year, in just the first half, 49 institutions were identified with recovery decisions totaling 429.1 billion won. Notably, the recovery amount per institution was less than 2 billion won five years ago, but last year it rose to 7 billion won, and this year it is about 8.8 billion won, showing a significant increase. This means that the fraudulent claim amount per individual office-head hospital has increased nearly fivefold over five years.
Conversely, the actual collection rate after recovery decisions for fraudulent claims at illegal medical institutions has plummeted. In 2018, the amount actually collected after recovery decisions was 28.3 billion won, with a collection rate (collected amount/recovery decision amount) of about 7.7%, but last year it was only 2.5% (23.6 billion won), and this year it is just 2.6% (11.2 billion won). Over the past five years, the total collected amount was 115.6 billion won, with a collection rate of about 4.4%.
In the case of office-head hospitals, the methods have become more sophisticated, making detection difficult, and the failure to recover fraudulent claims promptly is due to the lack of conditions for swift response. Since it is a specialized field, frontline police find investigations difficult, and even after receiving suspicious reports, follow-up actions are delayed. There have been ongoing criticisms for years that authorities’ responses are inadequate, such as failing to shut down the facilities in advance. During the 20th National Assembly, a bill was proposed to allow the National Health Insurance Service to appoint special judicial police officers, but it did not pass.
Assemblyman Choi Jong-yoon stated, "Medical benefit payments are leaking like blind money due to illegal medical institutions such as office-head hospitals," and emphasized, "The National Health Insurance Service must prioritize ensuring that medical benefits are properly paid and devise measures to increase the recovery rate of fraudulent medical benefits."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.
!["The Woman Who Threw Herself into the Water Clutching a Stolen Dior Bag"...A Grotesque Success Story That Shakes the Korean Psyche [Slate]](https://cwcontent.asiae.co.kr/asiaresize/183/2026021902243444107_1771435474.jpg)















