A new treatment method has been developed that awakens dormant immune cells (macrophages) inside tumors to attack cancer cells. The key is to restore the function of immune cells that are not performing their roles, thereby enhancing the therapeutic effect from within the tumor.
On December 30, KAIST announced that a research team led by Professor Jiho Park from the Department of Bio and Brain Engineering has developed a treatment in which a drug is injected into the tumor, allowing the body's macrophages to absorb it and independently produce CAR (chimeric antigen receptor) proteins. This process transforms them into 'CAR-macrophages,' which are immune cells engineered to recognize and attack cancer.
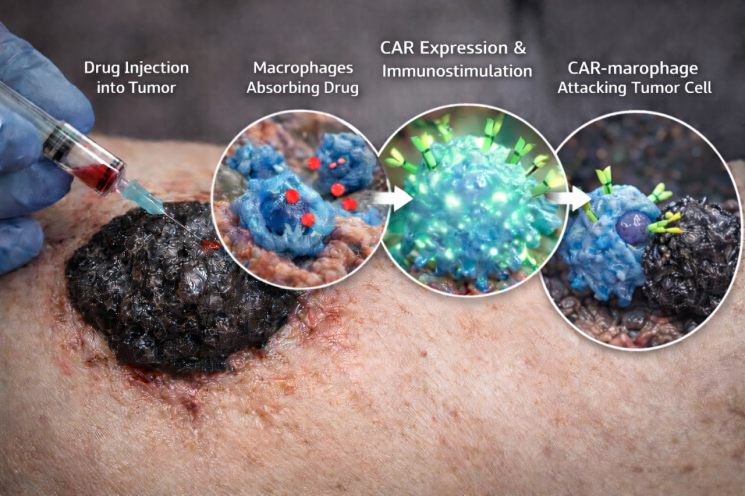 A new treatment method has been developed to awaken immune cells dormant inside tumors to attack cancer cells. Research schematic image generated by AI. Provided by KAIST.
A new treatment method has been developed to awaken immune cells dormant inside tumors to attack cancer cells. Research schematic image generated by AI. Provided by KAIST.
Solid tumors, such as gastric cancer, lung cancer, and liver cancer, grow as firm masses. Immune cells have difficulty infiltrating these tumors or maintaining their function inside them, which has limited the effectiveness of conventional immune cell therapies against solid tumors.
Recently, CAR-macrophages have gained attention as a next-generation immunotherapy because they not only directly engulf cancer cells but also activate surrounding immune cells, amplifying the anti-cancer response. However, CAR-macrophage therapy has required extracting immune cells from a patient's blood, culturing and genetically modifying them, which is both time-consuming and costly, and has posed significant challenges for actual patient application.
To address the difficulties of treating solid tumors and the burdens associated with CAR-macrophage therapy, the research team focused on 'tumor-associated macrophages' that are already present around the tumor.
The strategy involves using lipid nanoparticles, designed for easy absorption by macrophages, to deliver both mRNA containing cancer-recognition information and immune stimulants that activate immune responses. This approach aims to 'directly reprogram immune cells within the body.'
 Professor Jiho Park (left) from the Department of Bio and Brain Engineering, and Dr. Junhee Han (right). Provided by KAIST
Professor Jiho Park (left) from the Department of Bio and Brain Engineering, and Dr. Junhee Han (right). Provided by KAIST
The research team's strategy proved effective. When the therapeutic agent was injected into the tumor, macrophages rapidly absorbed it, produced proteins that recognize cancer cells, and activated immune signaling. The resulting 'enhanced CAR-macrophages' showed improved ability to eliminate cancer cells. Additionally, the activation of surrounding immune cells further boosted the anti-cancer effect.
When this method was applied in an animal model of melanoma (the most dangerous type of skin cancer), tumor growth was significantly suppressed, and the research team emphasized that the therapeutic effect could potentially extend beyond the local area to induce a systemic immune response.
Professor Park stated, "This study presents a new concept for immune cell therapy that generates anti-cancer immune cells within the patient's body (tumor). Most importantly, it is significant because it simultaneously overcomes the two main obstacles of conventional CAR-macrophage therapy: 'delivery efficiency' and the 'immunosuppressive environment.'"
Meanwhile, Dr. Junhee Han from the Department of Bio and Brain Engineering at KAIST participated as the first author of this study. The research results (paper) were recently published in the international journal 'ACS Nano' in the field of nanotechnology.
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.

![Clutching a Stolen Dior Bag, Saying "I Hate Being Poor but Real"... The Grotesque Con of a "Human Knockoff" [Slate]](https://cwcontent.asiae.co.kr/asiaresize/183/2026021902243444107_1771435474.jpg)














