Financial Supervisory Service, Seoul Police, and National Health Insurance Service Join Forces
1 Billion Won in Public Insurance and 400 Million Won in Private Insurance Fraud Uncovered
The Financial Supervisory Service announced on October 14 that, in cooperation with the Seoul Metropolitan Police Agency and the National Health Insurance Service, it apprehended a hospital director and 130 patients this month for defrauding public and private insurance companies of 1.4 billion won.
The director of Hospital B at Clinic A in Seoul administered nutritional IV therapies-such as combinations of “Cinderella” and “Baekok” drips-and cosmetic procedures like fillers and Botox to local residents. The director then issued and provided false medical records for manual and pain therapy treatments.
The hospital operated by selling packages such as 10 prepaid sessions for 2.1 million won, deducting visits as they were used for various nutritional IVs and cosmetic procedures. The dates and number of sessions for each prepaid patient’s IV and skincare treatments were meticulously recorded and managed in Excel files.
The majority of the 130 patients were residents of District A. Although they received nutritional IVs and cosmetic procedures, the records were falsified to appear as if they had received pain and manual therapy. These falsified records were submitted to insurance companies multiple times, allowing them to fraudulently claim 400 million won in indemnity (private) insurance payouts.
For example, Patient D, born in 1972, claimed to have received 43 sessions of lumbar physical and manual therapy from January 2021 to May 2023 and collected 8 million won in insurance payouts. However, it was revealed that this patient had actually received 44 sessions of nutritional IVs, Botox, and fillers for cosmetic purposes.
The hospital was also complicit. It disguised cosmetic procedures as pain injections (nerve blocks) and X-ray examination fees, then filed claims with the National Health Insurance Service, defrauding approximately 1 billion won in public health insurance benefits.
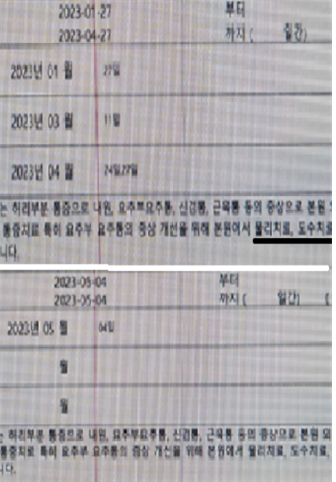 False medical records stating that the patient received nutritional IV therapy and skin treatments followed by lumbar physical and manual therapy. Financial Supervisory Service
False medical records stating that the patient received nutritional IV therapy and skin treatments followed by lumbar physical and manual therapy. Financial Supervisory Service
The Financial Supervisory Service warned that not only hospitals that orchestrate such crimes but also patients who participate are considered accomplices and are frequently subject to criminal penalties. Under the Special Act on Prevention of Insurance Fraud, violators can face up to 10 years in prison or a fine of up to 50 million won.
A representative from the Financial Supervisory Service stated, "Insurance fraud undermines the foundation of the insurance system and is a representative financial crime that harms the livelihoods of ordinary citizens by causing increases in premiums for the general public. The Financial Supervisory Service, the police, and the National Health Insurance Service will continue to actively cooperate to eradicate insurance fraud."
Insurance fraud can be reported by phone, through the Financial Supervisory Service website, or by mail. The 'Insurance Fraud Reporting Center' on insurance company websites can also be used.
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.

















