Most Specialists Quit Severe Trauma Care Midway Despite Over 380 Certified
Compensation Fails to Match Workload... Staffing Shortages Create a Vicious Cycle
Patients brought in bloodied from unexpected accidents, doctors fighting desperately against time to save fading lives, and a small number of medical staff efficiently triaging and treating patients even in extreme situations with a flood of casualties from major accidents... The Netflix web novel drama 'Severe Trauma Center' depicts the struggles of trauma surgeons, reflecting the ongoing harsh reality and hardships faced by severe trauma centers. Superhero trauma specialists like the drama's protagonist 'Baek Kang-hyuk' are rare in reality, and it is difficult to find junior doctors who are inspired by such portrayals and willingly volunteer to work in severe trauma centers.
Every year, the number of specialists giving up on dedicated severe trauma care is increasing. In 2011, Professor Lee Guk-jong of Ajou University Trauma Surgery gained nationwide attention by saving Captain Seok Hae-gyun, who was severely injured during the 'Aden Bay Dawn Operation,' sparking great interest in trauma surgery, but that interest was short-lived. Due to chronic manpower shortages, intense working hours, and the risk of medical accidents, trauma surgery is perceived as an undesirable specialty, and many regional trauma centers fail to fulfill their roles.
 A scene from the recently aired Netflix drama "Severe Trauma Center," where the main character Professor Baek Kang-hyuk (played by Ju Ji-hoon) boards a helicopter to save a patient. Provided by Netflix
A scene from the recently aired Netflix drama "Severe Trauma Center," where the main character Professor Baek Kang-hyuk (played by Ju Ji-hoon) boards a helicopter to save a patient. Provided by Netflix
Most Specialists Quit Midway Even After Completing Severe Trauma Training
According to the Ministry of Health and Welfare and the Korean Society of Trauma on the 17th, 13 specialists applied for and all passed the trauma subspecialty exam held on the 8th. Trauma subspecialists are surgeons specializing in trauma-related fields such as general surgery, neurosurgery, and cardiothoracic surgery, who undergo an additional two years of trauma training at 27 designated training hospitals nationwide and then qualify after evaluation. Since 2010, an average of 25 to 26 trauma subspecialists have been certified annually, totaling 371 by last year.
However, as of February 2025, only about 188 doctors are working as dedicated trauma specialists in medical settings, which is less than 200 nationwide. While new applicants are decreasing, the number of doctors who have obtained trauma subspecialty certification but later quit is increasing. The trauma subspecialty certification must be renewed every five years, but this year only 20.7% of those eligible for renewal applied, marking the lowest rate ever.
The reason for this attrition is that compensation does not match the harsh working conditions. The Ministry of Health and Welfare increased the salary for 'dedicated specialists at regional trauma centers' from 144 million KRW last year to 160 million KRW this year, but it still falls short of the average annual salary of 236 million KRW for all specialists (based on 2020). Although circumstances vary by hospital, trauma surgery generally does not contribute to hospital profits, resulting in insufficient treatment and support for medical staff. Hospitals with manpower shortages fall into a vicious cycle where remaining staff must work even harder.
Problems also arise from a lack of understanding and support for trauma surgery within hospitals. Trauma centers must keep separate spaces reserved for severe trauma patients who may arrive suddenly at any time. The number of patients that can be treated at once is limited, and if beds in the trauma center are occupied by relatively mild cases, the center cannot respond when a critical patient arrives. Due to the nature of trauma centers, there may be times with no patients and times with a sudden influx, but some hospital executives do not try to understand this emergency medical characteristic. A doctor at a regional trauma center said, "Unlike in the drama, it is rare for hospital directors to openly criticize the trauma center for deficits or performance, but when we complain about staffing or ICU shortages, they irresponsibly respond with 'It can't be helped' or 'Other hospitals are the same,' so we no longer even bring it up."
Regional Trauma Centers Failing to Fulfill Emergency Medical Responsibilities
Since regional trauma centers responsible for each area nationwide were designated in 2014, South Korea's 'preventable trauma mortality rate' has dropped from 35.2% in 2011 to 13.9% in 2021, less than half. Regional trauma centers are specialized trauma treatment centers prepared to provide emergency surgery and optimal care immediately upon hospital arrival for severe trauma patients with multiple fractures and bleeding caused by traffic accidents or falls. The significant reduction in the proportion of deaths that could have been prevented with timely and appropriate treatment indicates that if trauma centers are equipped with sufficient facilities, equipment, and personnel, mortality rates can be substantially lowered.
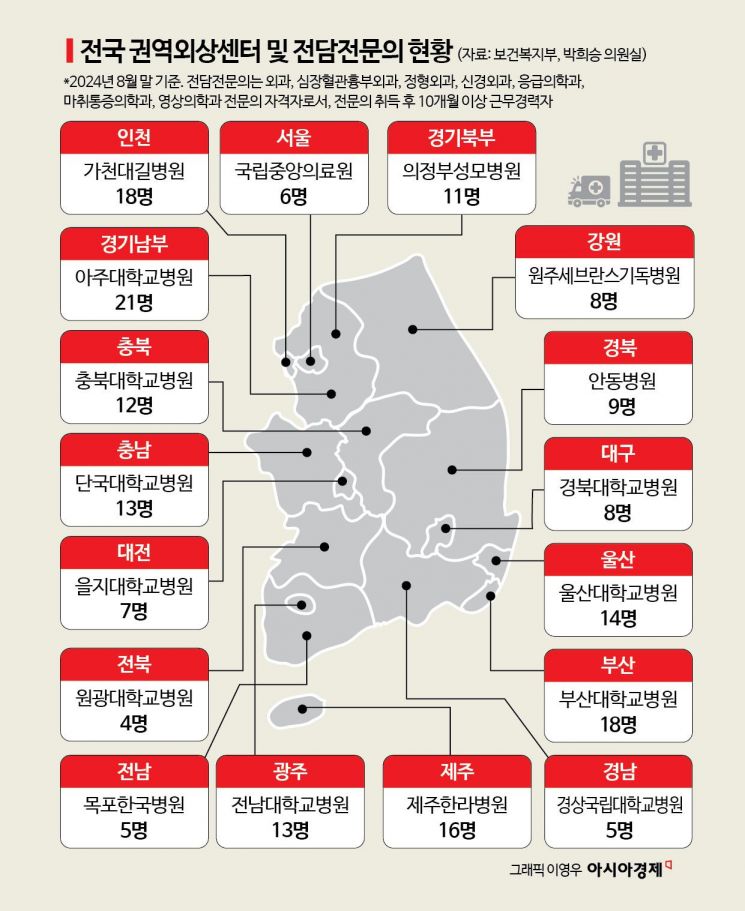
However, while all centers initially filled the required 23 to 27 specialists, over time, as the perception of low compensation relative to workload spread, manpower shortages worsened. As of August last year, among 17 regional trauma centers nationwide, only Ajou University Hospital in the southern Gyeonggi region had more than 20 dedicated specialists. Some trauma centers barely maintained operations with 4 to 5 doctors working almost every night, but due to ongoing conflicts between medical staff and government, they can no longer sustain normal operations. If trauma centers fail to meet the required medical personnel regulations, promised government funding will be cut. Therefore, rather than uniformly allocating government budgets to all regional trauma centers, there are opinions that support should be concentrated on centers with superior capabilities.
Cho Hang-ju, chairman of the Korean Society of Trauma and head of the trauma center at Uijeongbu St. Mary's Hospital, said, "For regional trauma centers to fulfill their roles, more doctors must be secured to operate under a stable system, but this is difficult under current conditions," and added, "Various incentives are needed to encourage doctors to choose to work at regional trauma centers given the demanding nature of the work." Im A-ram, director of the Disaster Medical Policy Division at the Ministry of Health and Welfare, explained, "We are currently reviewing plans to establish differentiated support and exit criteria based on evaluations of each regional trauma center through research projects. However, since regional trauma centers serve as key bases responsible for regional emergency medical care, any decision to suspend operations at a specific trauma center requires thorough consideration."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.