Public and Private Insurance Fraud of 7.2 Billion KRW
141 Medical Staff and Fake Patients Arrested
A group involved in insurance fraud by submitting false medical records at a residential nursing hospital was caught embezzling a total of 7.2 billion KRW in insurance payments. It was revealed that they took not only insurance payouts from insurance companies but also nursing care benefits from the National Health Insurance Service (NHIS), which covers part of the medical expenses.
According to the Financial Supervisory Service, Namyangju Northern Police Station, and NHIS on the 18th, 141 people, including five hospital medical staff and 136 patients, were arrested last month for orchestrating organized insurance fraud using a residential nursing hospital and embezzling both public and private insurance payments.
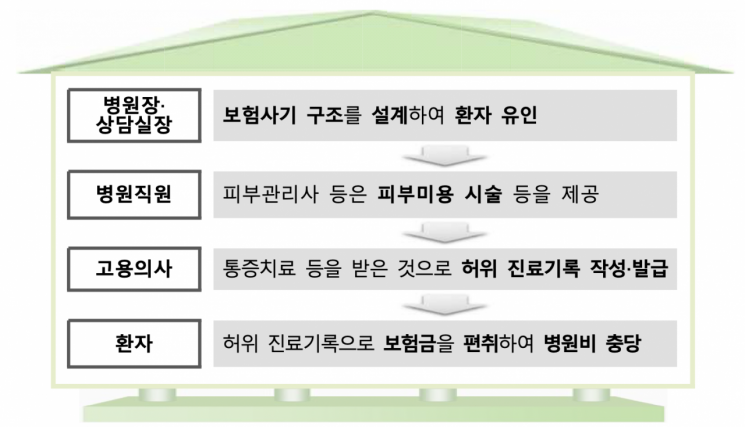
The hospital director and the counseling manager persuaded patients capable of daily living to be admitted, misleading them by saying they could receive cosmetic procedures within the insurance product coverage limits. They designed false treatment plans consisting of pain treatment, radiofrequency therapy, and medications so that insurance claims of about 5 to 6 million KRW per month could be made, while actually providing skin care treatments such as whitening and wrinkle improvement. If cosmetic procedures were not immediately necessary, services like 'storage' or 'transfer to others' were also available. When the inpatient treatment coverage limit was exhausted, false medical records were created to appear as if outpatient treatment had been received.
During this process, it was discovered that the hospital operated beyond the authorized number of beds to increase the number of long-term inpatients who paid high medical fees. The Ministry of Health and Welfare limits hospitals to operate 35 beds per doctor when granting hospital establishment permits. It was also revealed that counseling managers or hospital staff wrote medical records using doctors' IDs.
Using this method, the hospital covered a total of 6 billion KRW in embezzled indemnity insurance payments from May 2021. About ten patients embezzled amounts ranging from 100 million to 190 million KRW each. Additionally, they obtained another 1.2 billion KRW by fraudulently claiming inpatient fees and meal costs from the NHIS.
A Financial Supervisory Service official stated, "Not only the hospitals leading the insurance fraud but also patients who were tempted and participated have been criminally punished in many cases, so special caution is needed to avoid involvement in insurance fraud." They added, "Insurance fraud undermines the foundation of the insurance system and causes premium increases for honest citizens. Therefore, the Financial Supervisory Service, the National Police Agency, and the NHIS will continue to actively cooperate to eradicate insurance fraud."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.


![Clutching a Stolen Dior Bag, Saying "I Hate Being Poor but Real"... The Grotesque Con of a "Human Knockoff" [Slate]](https://cwcontent.asiae.co.kr/asiaresize/183/2026021902243444107_1771435474.jpg)















