Financial Supervisory Service Collaborates with Busan Police Agency to Uncover 1 Billion KRW Insurance Fraud
Double Ledger Used for List Management... False Receipts Issued for Treatments Like Dosu Therapy
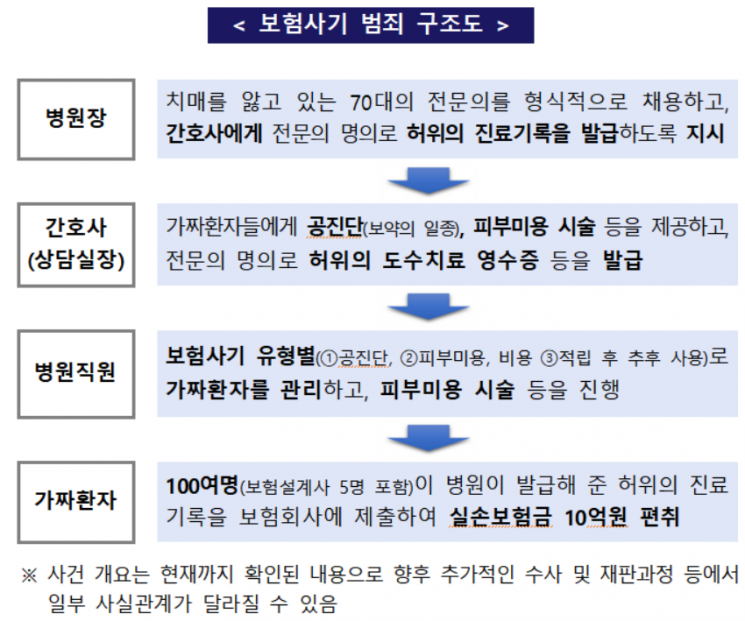
A gang involved in insurance fraud worth billions of won, consisting of a hospital director who is a Korean medicine doctor, nurses, hospital staff, and fake patients, has been caught.
The Financial Supervisory Service announced on the 9th that, based on information obtained through the 'Insurance Fraud Reporting Center' and in cooperation with the Busan Metropolitan Police Agency, they arrested 103 members of an organized insurance fraud group who embezzled indemnity insurance payments using false medical records.
The hospital director, Korean medicine doctor A, formally hired elderly specialist B to issue false medical records such as manual therapy. A instructed C, the counseling manager and nurse, to create false prescription and medical records using B's name.
C was found to have actively encouraged patients visiting the hospital to commit insurance fraud. C arbitrarily used B's name to create and issue false medical receipts so that fake patients could claim indemnity insurance for manual therapy and other treatments. At the same time, C instructed hospital staff to provide herbal medicine (Gongjindan) and skin beauty treatments (such as whitening and wrinkle improvement) corresponding to the amount paid at the hospital. In messenger conversations between C and hospital staff, when C said, "Mr./Ms. 000 has two manual therapy sessions, but please substitute one session with skin beauty treatment," a hospital staff member replied, "On Wednesday, we will proceed with esthetic (skin beauty) and spa instead of manual therapy."
Hospital staff separately noted phrases such as "esthetic treatment instead of manual therapy" next to the names of fake patients to distinguish them from regular patients involved in insurance fraud. They meticulously managed dual ledgers by color-coding the manual therapy roster in Excel files according to types of insurance fraud, maintaining separate schedules for actual beauty treatments and false manual therapy sessions.
More than 100 fake patients, lured by medical staff, received Gongjindan and skin beauty treatments but submitted false manual therapy receipts issued fraudulently to insurance companies, embezzling 1 billion won in indemnity insurance (an average of 10 million won per person). An integrated fraud analysis system (IFAS) linkage analysis of over 100 fake patients suggested that 11 were family or acquaintances. Among them, five were insurance planners.
A Financial Supervisory Service official said, "This case is a visible achievement after signing a business agreement with the National Police Agency earlier this year to eradicate organized insurance fraud linked to hospitals and clinics. Not only the hospitals and brokers leading the fraud but also patients who sympathized with and participated in their tempting proposals have been criminally punished in many cases. Therefore, insurance policyholders should be especially cautious not to become involved in insurance fraud."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.