KAIST Research Team Develops '2nd Generation T-Cell Receptor Therapy'
A next-generation immuno-oncology treatment has been developed that offers hope to terminal cancer patients for whom all anticancer treatments have failed.
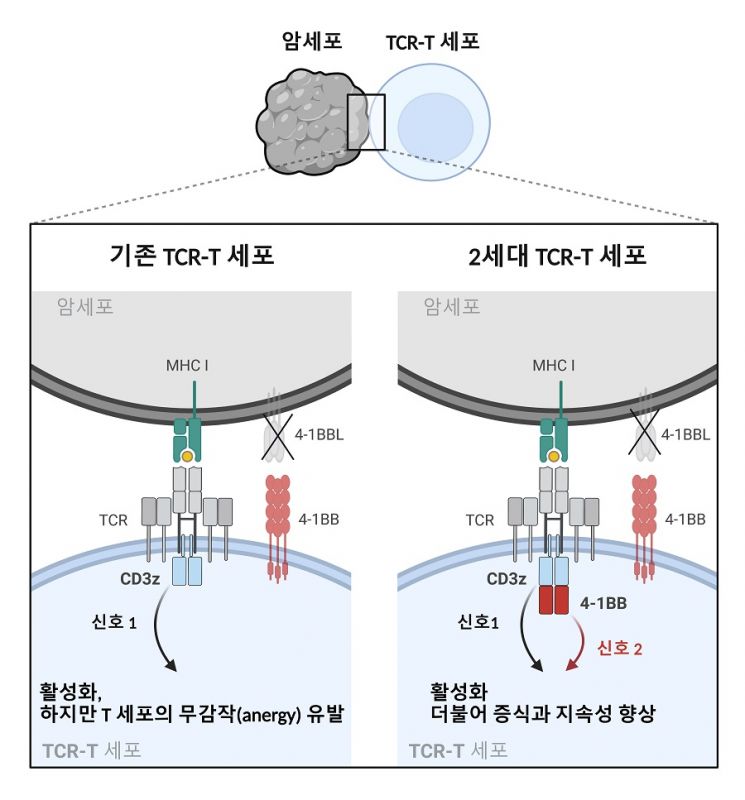
KAIST announced on the 20th that Professor Kim Chan-hyuk’s research team from the Department of Biological Sciences has developed a ‘second-generation T cell receptor-specific T (T cell receptor specific T·TCR-T) cell’ therapy that overcomes the tumor microenvironment which suppresses the immune system.
Cancer is considered a representative disease threatening the health of modern people. Among recent cancer research, the field that has made the most progress is immuno-oncology, which utilizes the immune system of cancer patients to overcome cancer.
The research team used CRISPR-Cas9 gene editing technology to produce TCR-T cell therapies that can directly destroy cancer cells through genetic manipulation. They improved the key CD247 gene involved in T cell receptor signaling by including an additional signaling domain that binds to TRAF2. This gene editing enhancement improved the proliferation and persistence of TCR-T cells, and demonstrated excellent anticancer effects in a malignant melanoma model using mice.
The results of this study were published on the 5th in the international journal Journal for Immunotherapy of Cancer.
Unlike first-generation chimeric antigen receptor (CAR) T cells, which showed limited initial anticancer effects, second-generation CAR-T cells containing additional signaling domains have shown over 80% high therapeutic efficacy in terminal leukemia patients and are called ‘miracle anticancer drugs.’ However, current CAR-T therapies are limited to treating blood cancers such as B-cell acute lymphoblastic leukemia and multiple myeloma. The lack of CAR-T therapies showing high efficacy in solid tumor patients remains a challenge to be addressed. Additionally, TCR-T therapies remain at the first-generation structural level, unlike CAR-T therapies.
The research team developed a second-generation TCR-T cell therapy targeting solid tumors that includes an additional signaling domain binding to TRAF2. Unlike CAR, which is composed of a single protein, engineering TCR?which forms a protein complex?to include additional signaling domains is much more challenging. After various attempts, the researchers established an optimal TCR module that induces additional signaling without affecting TCR formation and existing signaling.
Dr. Na Sang-jun, the first author, stated, “In the immunosuppressive environment formed by solid tumors, the anticancer effect of existing first-generation TCR-T cells is inevitably limited. On the other hand, second-generation TCR-T cells are designed with a technological strategy to maintain continuous anticancer effects even in immunosuppressive environments, and are expected to become necessary therapies for solid tumor patients for whom existing treatments are difficult to expect efficacy.”
(Paper title: Engineering second-generation TCR-T cells by site-specific integration of TRAF-binding motifs into the CD247 locus)
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.
![Clutching a Stolen Dior Bag, Saying "I Hate Being Poor but Real"... The Grotesque Con of a "Human Knockoff" [Slate]](https://cwcontent.asiae.co.kr/asiaresize/183/2026021902243444107_1771435474.jpg)















