Ministry of Health and Welfare Announces 'Essential Medical Support Measures'
[Asia Economy Reporter Lee Gwan-ju] The emergency medical system is being reorganized to ensure that essential medical services can be received anytime and anywhere, and the 'Public Policy Fee' will be officially introduced to strengthen compensation for essential medical care. Measures to expand the medical infrastructure will also be implemented to enhance access to childbirth and pediatric care, which have recently emerged as social issues.
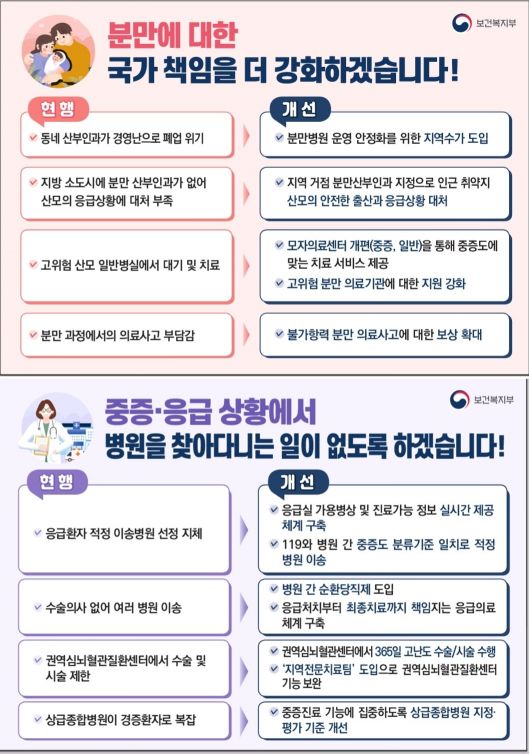
The Ministry of Health and Welfare announced on the 31st the finalized 'Essential Medical Care Support Measures' with these contents. This plan presents three main directions to establish a system that provides essential medical care needed by all citizens anytime and anywhere, focusing on severe emergency care, childbirth, and pediatric treatment: ▲ Establishing a regionally comprehensive essential medical care delivery system ▲ Introducing the Public Policy Fee ▲ Securing sufficient medical personnel.
Final Treatment of Emergency Diseases at Emergency Medical Centers... Expansion of Pediatric Care Infrastructure
The emergency medical system will be reorganized to be responsible for final treatments such as surgeries. To this end, the designation criteria for regional emergency medical centers will be revised to include final treatment functions for major severe emergency diseases, transforming them into severe emergency medical centers equipped with severe emergency treatment capabilities. After reorganization, the number of severe emergency medical centers will be expanded from the current 40 to around 50-60, and only institutions designated as severe emergency medical centers will be eligible to be designated as disease-specific specialized centers, thereby strengthening the linkage between emergency rooms and follow-up care.
Regional cardiovascular and cerebrovascular centers will be reorganized from their current focus on prevention and rehabilitation to specialize in advanced surgeries and treatments, ensuring that high-risk cardiovascular and cerebrovascular patients can undergo surgery within the golden hour (within 2 hours). Additionally, tertiary general hospitals will have their designation and evaluation criteria improved so they can focus on their core function of severe care, and their severe, emergency, and pediatric emergency treatment functions will be strengthened.
Measures to have major emergency diseases handled within one region are also being promoted. Through pre-established regional cooperation systems, medical institutions will operate a rotating on-call system for major emergency diseases and share this with 119 emergency services, so patients can be transported to the on-call hospital when emergencies occur. The Ministry of Health and Welfare explains that this aims to prevent ambulances from wandering without a hospital to accept patients by ensuring that at least one hospital in the region has an on-duty doctor at all times.
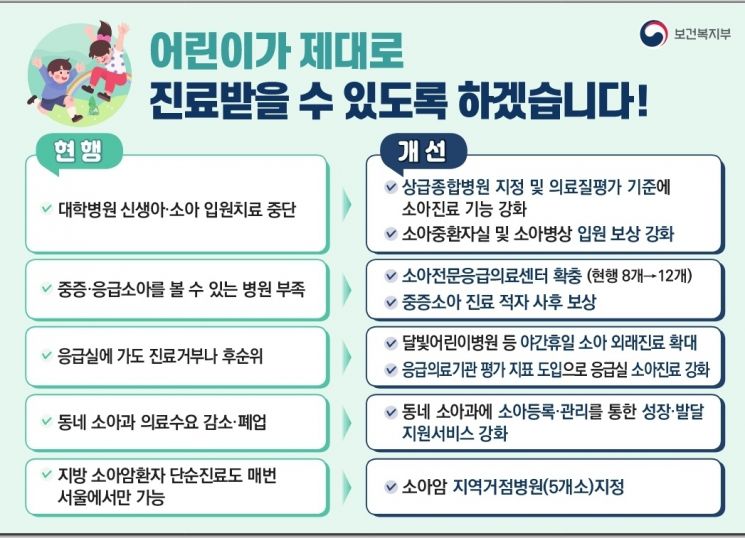
The medical infrastructure for pediatric patients, which has recently become a social issue, will also be expanded. Five new regional pediatric cancer base hospitals will be designated to activate collaborative treatment and recovery with existing children's public specialized treatment centers, establishing a treatment system so that pediatric cancer patients and their families in provinces do not have to travel to Seoul for necessary care. Additional pediatric specialized emergency medical centers will be expanded, and pediatric care institutions operating at night and on holidays (such as Moonlight Children's Hospitals) will be increased.
Introduction of Public Policy Fee... Focused Support for Severe Medical Infrastructure
The most notable part of this plan is the Public Policy Fee. It is a new health insurance compensation system designed to complement the limitations of the current fee-for-service system, focusing on strengthening infrastructure for high-level severe medical care and supporting the maintenance of infrastructure in fields struggling due to low demand.
First, compensation will be expanded in essential medical fields where medical personnel face heavy workloads such as night and holiday shifts and long waiting times. Compensation for emergency surgeries and procedures during nights and holidays for conditions like cerebral aneurysms and severe trauma will be increased compared to weekday daytime rates, and a new emergency-dedicated inpatient room management fee will be established to secure inpatient rooms for severe patients visiting emergency rooms and enable rapid linkage to follow-up care.
Additionally, a pilot project to retrospectively compensate children's public specialized treatment centers, which are specialized institutions for severe pediatric care, for their medical losses at the institutional level will begin this year. Compensation for relatively undervalued inpatient and surgical fields will also be strengthened, with additional support for high-level, high-risk surgeries.
Furthermore, a differentiated 'regional fee' will be introduced for the first time. Initially, regional fees will be provided to childbirth medical institutions located in cities and counties that meet certain facility and personnel standards to improve their operational difficulties. The effectiveness will be evaluated later to consider expanding this to other fields such as emergency and severe pediatric care. A 'Safety Policy Fee' will also be paid to create a safe childbirth environment, including the prevention of medical accidents.
Regarding pediatric care, efforts will be made to maintain pediatric inpatient care infrastructure by increasing neonatal unit inpatient fees at hospital and clinic levels, improving age-based surcharges for pediatric general ward admissions, and enhancing pediatric intensive care unit inpatient fees.
Improving Working Conditions and Expanding Medical Personnel
Measures to secure sufficient essential medical personnel have also been introduced. By analyzing work conditions and personnel supply and demand forecasts by field and region, improvements will be pursued in systems related to doctors' on-call and working hours, such as continuous resident work. At the same time, plans to alleviate the criminal liability burden on medical personnel for unavoidable medical accidents and to strengthen support for victims of medical accidents will be reviewed. To reduce personnel disparities between regions and essential specialties, measures to expand the placement of residents in provincial hospitals and essential specialties will be implemented. The Ministry of Health and Welfare plans to adjust the quota for specialized fields but will first establish principles for quota allocation by specialty.
To minimize problems such as the outflow of essential medical personnel to the rapidly expanding non-reimbursed medical market, important non-reimbursed items will provide not only price information but also safety and efficacy information. Monitoring of non-reimbursed medical practices, joint inspections, and discussions on improving related payment standards will be strengthened, along with linked management with indemnity insurance.
Additionally, essential medical education and training will be strengthened during the medical personnel training process, and specific implementation plans will be prepared through consultations with the medical community to ensure adequate medical personnel are secured to address regional doctor shortages and imbalances in essential fields. Minister of Health and Welfare Cho Kyu-hong stated, "Strengthening the foundation of essential medical care is a national task that must be continuously developed, and this plan is the first step in strengthening the essential medical care foundation." He added, "We will continue to supplement the plan by preparing additional measures for necessary fields in the future."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.
!["The Woman Who Threw Herself into the Water Clutching a Stolen Dior Bag"...A Grotesque Success Story That Shakes the Korean Psyche [Slate]](https://cwcontent.asiae.co.kr/asiaresize/183/2026021902243444107_1771435474.jpg)















