①Increase Vaccination Rates
②Protect Nursing Hospitals and Facilities
③Secure ICU Beds
As the resurgence of COVID-19 began earlier than initially expected, concerns are growing that severe cases and deaths will surge, especially among the elderly. Analysts point out that the combination of low vaccination rates, waning immunity, and the seasonal characteristics ahead of winter increases the likelihood of infections worsening into severe conditions. Experts urge immediate encouragement of additional vaccinations for vulnerable groups and strengthening infection control measures in nursing hospitals and facilities to minimize the damage caused by the spread.
Immune Effect Expected Two Weeks After Vaccination
According to health authorities and infectious disease experts on the 16th, after the sixth COVID-19 resurgence peaked in mid-August and began to decline in late October, the seventh resurgence started again within just 2 to 3 weeks, making long-term predictions about the COVID-19 situation increasingly difficult. Until early September, the seventh resurgence was expected to begin between late December and January or February of next year, but it started more than a month and a half earlier.
Moreover, unlike other countries overseas where new waves were expected to be driven not only by the Omicron subvariant 'BA.5' but also by other derived subvariants such as 'BQ.1' and 'BQ.1.1,' recent variant detection rates show that BA.5 is still leading the wave domestically.
Professor Kim Tak of the Department of Infectious Diseases at Soonchunhyang University Bucheon Hospital explained, "Until now, Korea's COVID-19 trends tended to follow other countries' cases, but recently, each country is showing different epidemic patterns. The fact that BA.5, rather than other immune-evasive variants, remains dominant domestically suggests that people who have not been previously infected are newly contracting the virus."
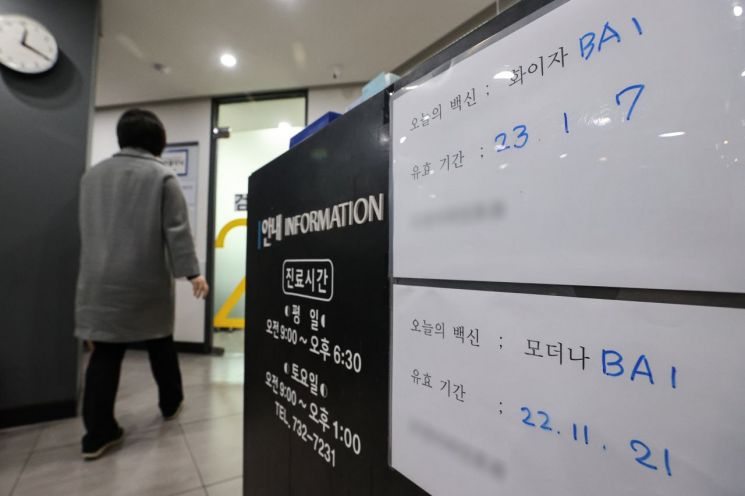
With winter approaching?a season favorable for virus activity?and immunity from vaccination or infection at its lowest, health authorities have hastened to promote winter vaccinations, but public response remains low, which is also cited as a factor in the spread. Fatigue from repeated vaccinations has accumulated, and those with a history of infection tend to believe they have sufficient immunity, leading to a reduced sense of urgency about COVID-19 compared to before. Although the updated vaccine campaign began over a month ago on the 11th of last month, the winter vaccination rate among those aged 60 and older is only 10.8%, and among those in their 60s who need additional doses after four months since their last vaccination, the rate is just 12.6%.
Professor Jung Jae-hoon of the Department of Preventive Medicine at Gachon University College of Medicine said, "The peak of this resurgence will be as early as the end of this month or at the latest early December. Since it takes at least two weeks after vaccination to expect sufficient immune protection, people should hurry to get vaccinated."
Higher Proportion of Severe Cases and Deaths Among Confirmed Patients
On the other hand, experts diagnose that compared to the early phase of the sixth resurgence, the proportion of severe cases and deaths among new confirmed cases has generally increased since the start of the seventh wave. In the week immediately after the government officially declared the seventh wave (November 9?15), there were 371,785 new confirmed cases, 356 deaths, and an average of 371 severe cases per day. In contrast, during the week when the sixth resurgence began (July 13?19), there were 299,661 confirmed cases, 99 deaths, and an average of 73 severe cases per day.
Professor Kim said, "Compared to previous waves, mild patients may have been less likely to undergo COVID-19 diagnostic testing, which could have increased the proportion of severe cases relative to confirmed cases. Also, as the vaccine's effectiveness in preventing severe illness decreases, the rate of severe cases among the elderly may have risen. We believe both factors are influencing the situation on the ground."
Professor Eom Jung-sik of the Department of Infectious Diseases at Gachon University Gil Medical Center pointed out, "Although the COVID-19 vaccines developed so far have limitations in providing long-term protection, they remain the only preventive measure to protect high-risk groups. If vaccination rates remain low, not only will face-to-face visits to nursing hospitals and facilities need to be restricted again, but infection control measures for staff will also have to be strengthened during the progression toward the epidemic peak."
While frontline hospitals are transitioning to treat COVID-19 patients within the general medical system, preparations are also needed in case more severe cases occur in the future. As of the 14th, the nationwide utilization rate of 1,575 severe care beds is 34.0%, indicating some capacity remains, but for semi-severe beds, more than half?1,302 out of 2,471?are in use. Professor Eom emphasized, "Since influenza and respiratory infections continue to occur, and severe patients with cardiovascular diseases increase in winter, if the surge in severe COVID-19 cases coincides with this, intensive care beds could become severely insufficient. We must prepare measures to quickly secure beds in advance."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.