Obesity as the Root Cause of Many Diseases, Classified as a Condition Requiring Long-Term Treatment
A 2013 US JAMA Published Paper First Proposed This
"People Considered Overweight Have Lower Mortality Risk"
Active Research on the Obesity Paradox Related to Cancer Also Underway in Korea
[Asia Economy Reporter Lee Gwan-joo] Obesity is considered a "root of all diseases" alongside smoking, stress, and excessive drinking. The World Health Organization (WHO) classified obesity as a disease requiring long-term treatment in 1997, and since then, obesity has been recognized as a major disease that must be addressed from a global public health perspective. In fact, the medical community reports that obese patients have a 1.5 to 2 times higher risk of coronary artery disease, 2.5 to 4 times higher risk of hypertension, and 5 to 13 times higher risk of diabetes compared to the general population. Additionally, obesity is known to cause various comorbidities in the gastrointestinal, respiratory, metabolic endocrine, musculoskeletal, and nervous systems.
Sixteen years after the WHO announcement, in January 2013, a brief paper that challenged this perception was published in the Journal of the American Medical Association (JAMA). The 12-page paper titled "Association of All-Cause Mortality With Overweight and Obesity Using Standard Body Mass Index Categories," authored by Dr. Catherine Flegal and her team at the U.S. National Center for Health Statistics (NCHS), first introduced the so-called "obesity paradox." The research team reported that people considered overweight had a 6% lower risk of death during the same period compared to those with normal weight.
Although some scholars initially opposed the findings, many supported the paper after analyzing extensive data from 97 prospective studies involving 2.88 million people that used BMI to evaluate mortality rates. However, this remains a hypothesis rather than a definitively proven fact. Currently, the medical community interprets this to mean that for some groups, such as middle-aged or older adults or those already ill, a slight increase in weight may not be particularly harmful and might even aid recovery.
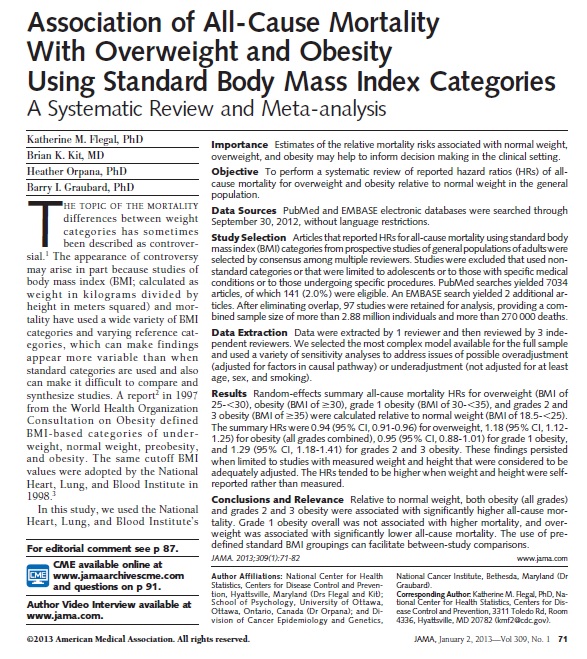 The paper published on January 2, 2013, in the Journal of the American Medical Association (JAMA), where the "obesity paradox" was first proposed.
The paper published on January 2, 2013, in the Journal of the American Medical Association (JAMA), where the "obesity paradox" was first proposed. [Photo by JAMA]
Notable research on the obesity paradox has also been conducted domestically this year, especially focusing on cancer. A research team led by Professors Lee Jong-hwan and Park Jeong-chan from the Department of Anesthesiology and Pain Medicine and Professor Lee Seung-hwa from the Department of Cardiology at Samsung Seoul Hospital tracked 87,567 cancer patients who underwent surgery between March 2010 and December 2019. They found that obese patients had a lower risk of death after cancer surgery compared to those with normal or underweight BMI. The mortality rate within three years post-surgery was 6.4%, with obese patients (BMI 25 or higher) having a 31% lower risk of death than normal-weight patients and 62% lower than underweight patients (BMI below 18.5).
Regarding these findings, the research team hypothesized that in cancer surgeries, which impose significant physical burdens, obese patients may have an advantage in recovering strength. Professor Lee Jong-hwan, who led the study, explained, "Since the analysis did not differentiate cancer types or stages, more detailed research is needed to accurately assess the impact of obesity. However, this study proves that cancer patients with body weight below an appropriate level before surgery tend to have poorer prognoses. Therefore, both patients and medical staff should carefully monitor such cases and actively engage in treatment."
Professor Kim Na-young’s team from the Department of Gastroenterology at Bundang Seoul National University Hospital also conducted a study analyzing the survival rates of 14,688 gastric cancer patients in relation to age, gender, and BMI. They confirmed that while prognosis improved progressively with extreme obesity (BMI 30 or higher) in men, this trend was not clearly observed in women. This indicates that the obesity paradox in gastric cancer manifests differently depending on gender. Professor Kim said, "If we study the differences in gastric cancer prognosis and patterns by gender more deeply, it will help clarify the exact mechanism of the obesity paradox and advance gastric cancer treatment methods."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.

















