Professor Seungpyo Lee of Seoul National University Hospital and Professor Dahee Kim's Research Team at Asan Medical Center
[Asia Economy Reporter Kim Young-won] A study has found that patients with primary mitral regurgitation who have specific clinical characteristics may have poor prognoses, indicating the need for caution in surgery. It is expected that predicting surgical outcomes of mitral regurgitation using clinical phenogroups discovered by domestic researchers will enable personalized treatment for patients.
A joint research team led by Professor Lee Seung-pyo of the Department of Cardiology at Seoul National University Hospital (Specialist Kwak Soon-gu) and Professor Kim Dae-hee of the Department of Cardiology at Asan Medical Center (Professor Lee Seung-ah) analyzed 2,321 patients with primary mitral regurgitation who underwent surgery at three large hospitals from 2006 to 2020 and identified five clinical phenogroups associated with surgical outcomes, the team announced on the 8th.
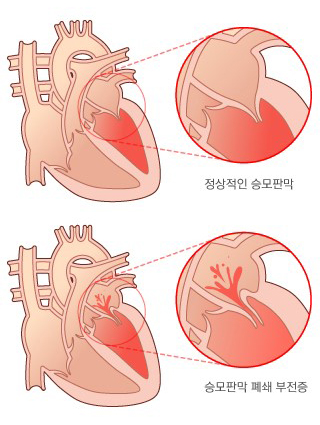
Mitral regurgitation is a condition in which the mitral valve does not close properly during heart contraction, causing blood to flow backward from the left ventricle to the left atrium. Primary mitral regurgitation refers to cases caused by abnormalities of the valve itself. When severe, it can lead to heart failure and sudden death, making accurate diagnosis and appropriate treatment planning crucial.
The only treatment is open-heart surgery to repair or replace the diseased valve. Recently, percutaneous valve repair procedures have been performed for patients who are difficult to operate on due to underlying conditions. Existing clinical guidelines from the US and Europe for these treatments have uniformly applied criteria for determining the appropriate timing of surgery to all patients.
The research team used latent class analysis to explore specific clinical patterns among patients to serve as guidelines for determining the appropriate timing and method of treatment. This technique classifies the entire sample into homogeneous subgroups. Because it classifies patient data based on observed patterns, it has the advantage of discovering unique disease patterns that deviate from existing clinical classification systems.
First, the team conducted latent class analysis on data from 1,629 patients at Asan Medical Center. As a result, five distinct clinical phenogroups were observed. The groups were classified as follows: Group 1 (patients with minimal comorbidities), Group 2 (males with severe left ventricular dilation), Group 3 (females with rheumatic valve regurgitation), Group 4 (low-risk elderly), and Group 5 (high-risk elderly). Groups 1 to 3 consisted of relatively younger patients.
Comparing 5-year postoperative survival rates, Group 5 (high-risk elderly) had the lowest rate at 83.4%, followed by Group 3 (91.7%) and Group 4 (95.6%). Similar patterns were observed in patients at Seoul National University Hospital and Bundang Seoul National University Hospital.
When the research team used these phenogroups to predict postoperative mortality, performance comparable to the internationally standardized risk score MIDA was observed. In other words, the team explained that these phenogroups have potential as universal risk prediction indicators.
For example, patients with minimal comorbidities (Group 1) had a very high 5-year postoperative survival rate of 98.5%, suggesting that early surgery can be actively considered even if asymptomatic. Conversely, high-risk elderly patients with many comorbidities (Group 5) had over 10% mortality within one year after surgery, indicating that percutaneous procedures may be more appropriate than surgery. Groups 3 and 4 also showed relatively low postoperative survival rates, requiring caution.
Specialist Kwak Soon-gu stated, "The study confirmed that diverse clinical clusters exist even among patients with mitral regurgitation."
Professor Lee Seung-pyo said, "It is expected that by establishing personalized treatment strategies based on the clinical characteristics and prognoses of the discovered phenogroups, precision medicine that benefits patients with valvular disease can be realized."
Meanwhile, this study was conducted with support from the Korea Health Industry Development Institute and was published in the latest issue of the British Medical Journal’s Heart.
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.