If Costs Surge or No Efficacy, 'Refund'
Measures for Managing High-Cost Treatments Also Established
Concurrent Benefit Assessment and Drug Price Negotiation to Shorten Time
Economic Evaluation Skipped if 'Target Patients Are Few'
[Asia Economy Reporter Lee Chun-hee] The national health insurance coverage for the ultra-high-priced treatment 'Zolgensma,' which costs about 2 billion KRW domestically, will be implemented starting next month. However, since the health insurance finances must bear the cost of over 1.9 billion KRW per administration, concerns continue to arise that the successive coverage of expensive rare disease treatments could deal a fatal blow to the already deteriorating health insurance finances. In response, the government plans to actively introduce a 'risk-sharing scheme' to prepare for cases where the actual drug efficacy significantly decreases or excessive claims are made despite the high cost, while also strengthening the management of high-priced treatments.
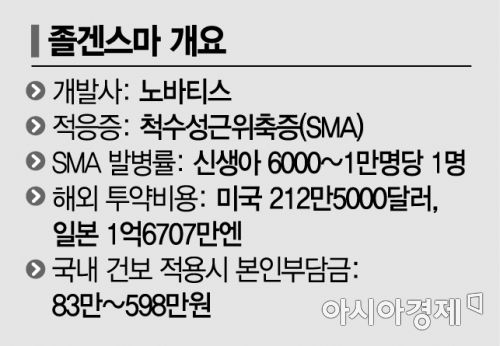
On the 20th, the Ministry of Health and Welfare held the 16th Health Insurance Policy Deliberation Committee meeting and announced that it had approved the revision of the drug benefit list and the benefit ceiling price table, including the new health insurance application for Zolgensma, a treatment for spinal muscular atrophy (SMA) by Korea Novartis. The revisions will be applied from next month after going through the relevant procedures.
With Zolgensma's domestic price set at 1,981.73 million KRW, the health insurance will bear about 1.98 billion KRW per administration. Due to the application of rare disease special cases and out-of-pocket maximum systems, the patient's actual burden is reduced to between 830,000 KRW and 5.98 million KRW. Considering the incidence rate, it is estimated that 20 to 30 patients will occur annually in Korea, resulting in an additional annual health insurance expenditure of around 40 billion KRW.
Introduction of 'Risk-Sharing Scheme'... Pharmaceutical Companies 'Refund' if Patient Numbers Surge or Drug Efficacy Declines
Conscious of such cost burdens, the government has introduced various risk-sharing schemes that share risks with pharmaceutical companies considering the actual efficacy and impact on insurance finances. For Zolgensma, three types of risk-sharing schemes?refund type, total amount cap type, and patient unit performance-based type?are specified in the contract with Novartis.
The refund type requires the pharmaceutical company to refund a certain percentage of the claimed amount to the National Health Insurance Service. The total amount cap type mandates that if the claimed amount exceeds a predetermined annual cap, the company refunds a certain percentage of the excess. The patient unit performance-based type tracks patient outcomes over five years; if treatment fails, the pharmaceutical company either fully covers the treatment cost or refunds part of the cost to the National Health Insurance Service. Previously, risk-sharing schemes such as total amount cap and patient unit performance evaluation were applied to the leukemia chimeric antigen receptor (CAR)-T cell therapy 'Kymriah,' which is also covered by health insurance. Additionally, in the fourth year after listing, clinical usefulness and cost-effectiveness are re-evaluated, leading to price adjustments and changes in refund rates.
Pre- and post-administration management procedures have also been established. Before administering Zolgensma, a prior written review is conducted to confirm eligibility according to the benefit criteria. Furthermore, the patient's guardian must sign a consent form agreeing to periodic response evaluations and long-term follow-up surveys for five years.
Cross-administration with the existing treatment 'Spinraza' is allowed under limited conditions. Among Spinraza-treated patients with SMA due to SMN1 deletion or mutation, cross-administration with Zolgensma is possible if the patient is under 24 months of age, weighs less than 13.5 kg, and started Spinraza before 12 months of age and continues to receive it. However, if other SMA treatments such as Spinraza are administered after Zolgensma, health insurance coverage for Zolgensma administration is not recognized.
Systematic Management... Rapid Introduction, Strict Economic Evaluation
The government, considering the increasing social demand for high-priced severe disease treatments, plans to promptly enhance accessibility while preparing measures to strengthen benefit management. Following Kymriah (360 million KRW) and Zolgensma, treatments such as the amyloid cardiomyopathy drug 'Vindamax' (200 million KRW annually), neurofibromatosis treatment 'Koselugo' (200 million KRW annually), and hereditary retinal disease treatment 'Luxturna' (1 billion KRW) are also aiming for insurance coverage.
The government defines high-priced drugs as 'drugs requiring price management and long-term effect verification due to high prices and uncertainty of efficacy.' Detailed criteria have been set for focused management, including so-called 'one-shot treatments' expecting long-term effects from a single treatment, drugs with annual financial requirements exceeding 300 million KRW per person, and drugs with annual health insurance claims exceeding 30 billion KRW.
To this end, three major management directions have been presented: ▲improving patient accessibility ▲strengthening monitoring of treatment efficacy and safety ▲enhancing benefit management.
First, to improve patient accessibility, a plan is underway to simultaneously conduct the Health Insurance Review and Assessment Service's drug benefit evaluation, which takes an average of 120 days, and the National Health Insurance Service's price negotiation, which takes 60 days. This aims to reduce the benefit review period from about 180 days to 120 days, shortening it by 60 days. For diseases with life-threatening conditions and no appropriate treatment methods, a pilot program will be conducted to concurrently perform drug benefit evaluation and pre-price negotiation simultaneously with the Ministry of Food and Drug Safety approval application.
Additionally, to alleviate the price burden and uncertainty of long-term effects of high-priced new drugs, the application of patient unit performance-based risk-sharing schemes will be gradually expanded.
To strengthen monitoring of treatment efficacy and safety, a system will be established to collect patient-specific administration and efficacy data for post-management of high-priced drugs. The usage-price linkage system, which adjusts prices for drugs with a certain level of increased drug costs, will also be improved.
Finally, to enhance benefit management, a 'prior authorization standard operating procedure (SOP)' will be established before administering ultra-high-priced drugs. The exemption from economic evaluation, currently applied only to rare diseases or anticancer drugs with no equivalent products or treatments, will be more strictly limited to cases with a 'small number of target patients,' and improvement measures for the exemption system will be prepared and supplemented.
The Ministry of Health and Welfare plans to coordinate these measures with the Health Insurance Review and Assessment Service, National Health Insurance Service, and Ministry of Food and Drug Safety and incorporate them into the 2nd Comprehensive Health Insurance Plan for 2024?2028.
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.