[With Corona Task - Part 2]
Ad Hoc Bed Mobilization Has Limits
"Must Increase at Least Twice from Now"
Chronic Shortage of Medical Staff
Asymptomatic and Mild Patients Practically 'Self-Isolate'
Focus Remaining Medical Capacity on Critical Care
Social Acceptance of 'Confirmed Cases Next Door' Is Key
To usher in the ‘with corona’ era where daily life coexists with COVID-19, the fatality rate of COVID-19 must be reduced to a level similar to that of the flu. In particular, it is pointed out that the healthcare system must be sufficiently reinforced, including expanding intensive care unit (ICU) beds and medical staff, in preparation for the possibility of an increase in critically ill patients. Along with this, experts argue that a social consensus should be established first to allow mild patients to stay at home and receive treatment.
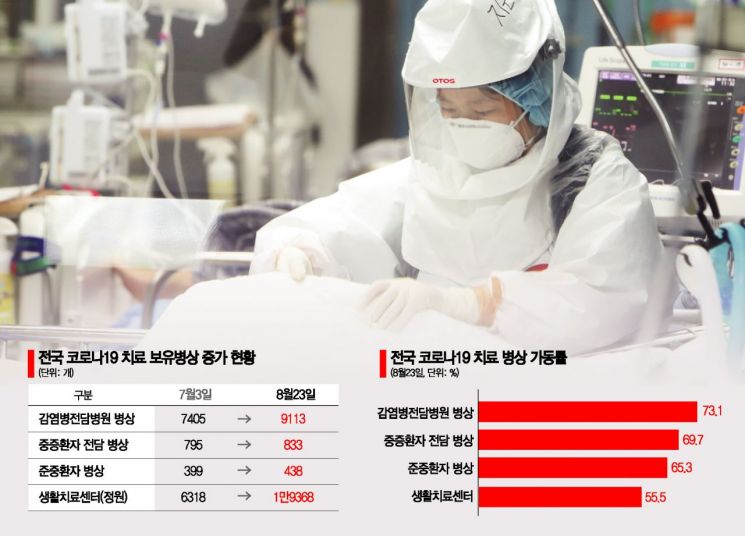
◆ Strengthening the healthcare system must precede with corona transition = According to the Central Disaster and Safety Countermeasures Headquarters, as of the 24th, the nationwide infectious disease-dedicated hospital bed occupancy rate reached 73.1%. The ‘dedicated ICU beds’ equipped with equipment and personnel for treating severe COVID-19 patients and designated by the Central Accident Response Headquarters were 69.7% occupied as of the 23rd, and the semi-ICU beds were 65.3% in use.
As the fourth wave, which intensified last month, continued to spread for over a month, the government hurriedly moved to expand beds. It was only on the 13th that an administrative order was issued to increase the mobilization rate of ICU beds in tertiary general hospitals to 1.5%. Accordingly, frontline medical institutions became busy, such as Seoul Asan Medical Center expanding beds for severe COVID-19 patients from 27 to 41. Authorities explain that the healthcare system can respond even if new confirmed cases occur within 2,500 per day.
However, if the transition to with corona occurs, the number of COVID-19 patients will be much larger than now, and the number of severe patients will inevitably increase. In fact, as the fourth wave continued, the number of severe patients hospitalized on this day reached 420, the highest since statistics began on March 28 last year. This is why there are criticisms that the current ad hoc bed mobilization has its limits.
Professor Eom Jung-sik of the Department of Infectious Diseases at Gachon University Gil Medical Center said, "To transition to with corona, ICU beds for severe patients must be secured at least twice as many as now," adding, "When considering only COVID-19 patients excluding ICU patients with other diseases, the capacity to fully accommodate those severe patients is necessary." Professor Kim Yoon of the Department of Healthcare Management at Seoul National University College of Medicine also emphasized, "Since severe patients can lead to death, priority must be given to securing ICU beds and preparing accordingly."
Expanding medical staff caring for COVID-19 patients is also urgent. Professor Kim said, "Medical personnel operate according to beds, but currently there is a chronic shortage of staff," and pointed out, "It is also necessary to review whether other medical personnel are being deployed to care for severe and emergency patients comparable to COVID-19 ICU patients." Professor Eom added, "It takes at least 2 to 3 years of work experience to properly treat ICU patients, but there is no time for training now," and suggested, "An alternative could be to gather medical staff who have ICU experience but are currently not working to build up the workforce."
◆ Mild patients treated at home? One of the major changes with the transition to with corona is that asymptomatic or mild patients who currently stay at residential treatment centers should, in fact, self-isolate at home. Increasing self-treatment would allow the remaining healthcare system capacity to focus on treating severe patients. There are also opinions that the current patient classification system, including severe patients, should be partially revised for efficient bed management. Professor Kim said, "The current high-flow oxygen therapy used to determine severity is not an appropriate criterion," and added, "Treatment should be organized according to actual severity."
This involves the issue of how socially acceptable it is. Jang Young-wook, a senior researcher at the Korea Institute for International Economic Policy, said, "After securing sufficient bed capacity, even if confirmed cases occur, the cost of controlling them is too high, so it is more efficient resource allocation to accept this as a quarantine policy," and argued, "Self-treatment also requires systems such as patient monitoring, but social consensus must be reached so that the public can accept having COVID-19 patients living next door."
Professor Eom also said, "In Korea, there is a tendency to take with corona too lightly," and added, "A social consensus is needed to accept possible problems that may arise when transitioning to with corona, such as sudden symptom worsening or an increase in deaths during self-treatment."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.