Deliberation on the Second-Year Implementation Plan of the National Health Insurance Comprehensive Plan
Establishing a Regionally Self-Sufficient Essential Medical System and Strengthening the Medical Safety Net
The government has decided to raise the fees for more than 2,000 medical procedures, including surgery, treatment, and anesthesia fees that have been relatively undervalued in essential medical fields such as pediatrics and emergency care, by 2027. Additionally, support for emergency abdominal surgeries at regional surgical hospitals will be expanded, and a pilot project to support regular and predictable shift work for nurses in vulnerable areas suffering from nurse shortages will be extended for another three years.
On the 27th, the Ministry of Health and Welfare held the '6th Health Insurance Policy Deliberation Committee Meeting of 2025' and reviewed the second-year implementation plan of the '2nd National Health Insurance Comprehensive Plan (2024?28),' which includes 75 detailed tasks for strengthening essential and regional healthcare and establishing a sustainable health insurance system.
Increase in Fees for Over 1,000 Essential Medical Surgeries and Anesthesia Procedures
According to the implementation plan, the government will first focus on raising fees for over 1,000 surgeries, treatments, and anesthesia procedures in the first half of this year to address the imbalance in health insurance fees for essential medical care. In particular, fees will be increased for high-difficulty and resource-intensive areas such as pediatrics and emergency care, with plans to rapidly raise fees for more than 2,000 undervalued procedures by 2027. The government will establish a fee determination structure linking the conversion factor and relative value points, prepare standardized cost calculation guidelines, and strengthen the cost survey foundation by expanding panel hospitals.
For severe pediatric surgeries, compensation for high-difficulty medical procedures such as age-based surcharges will be strengthened, and public policy fee support such as fees to maintain delivery infrastructure will be continuously promoted. The results of a pilot project for an alternative payment system that rewards based on medical quality and achievement of outcomes rather than volume will also be evaluated.
To build a regionally self-sufficient essential medical system, the government will support faculty salaries (26 billion KRW) and facilities and equipment (81.5 billion KRW) at regional base national university hospitals and regional general hospitals, provide low-interest loans (120 billion KRW) for other necessary funds to enhance capabilities, and strengthen the system for recovery-phase medical institutions, as well as chronic medical and nursing support systems to prepare for an aging society, including long-term care, nursing, and caregiving.
Efforts will also be made to solidify the medical safety net to eliminate blind spots in healthcare. Pilot projects for disabled and dental primary care physicians will continue, and access to medical care for vulnerable groups will be improved and financial burdens eased by expanding coverage for treatments of severe and rare diseases (expected 20 new cases and 10 expansions of coverage).
According to the '2nd Medical Reform Implementation Plan' announced on the 19th, non-covered services with high concerns of overuse will be temporarily applied as managed care for five years, after which their continuation will be decided through reevaluation. Non-covered services for cosmetic and plastic surgery purposes and those unnecessarily overlapping with covered services will be restricted.
Furthermore, essential medicines and therapeutic materials will be managed to ensure stable supply, and related systems will be improved to allow innovative new drugs and new medical devices to enter medical sites quickly. Additionally, the opening and utilization of health insurance data for public interest, scientific research, and self-directed health management will be expanded, and international cooperation related to health insurance systems and projects will be supported.
The Ministry of Health and Welfare stated, "Through the second-year implementation plan of the 2nd National Health Insurance Comprehensive Plan, we plan to strengthen essential medical care and achieve the goal of establishing a sustainable health insurance system without setbacks," adding, "We will also promote this more substantively in connection with reform tasks such as the 2nd Medical Reform Implementation Plan."
200% Additional Fee for 62 Emergency Abdominal Surgeries at Regional Surgical Hospitals
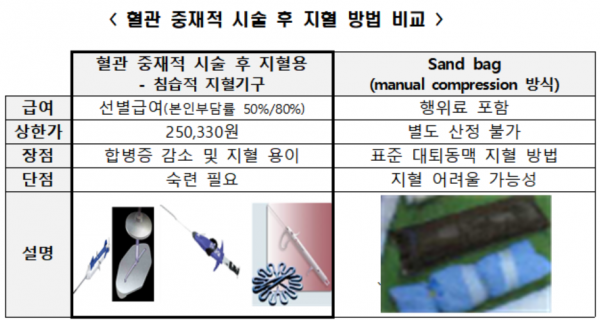
At the Health Insurance Policy Deliberation Committee meeting, it was also decided to convert the 'use of invasive hemostatic devices after vascular interventional procedures,' which is currently applied as selective coverage (50% or 80% patient co-payment), to essential coverage (20% patient co-payment, 5% with special calculation exception) when hemostasis is difficult. There had been criticism that invasive hemostatic device use, which reduces complications and has therapeutic effects for patients requiring rapid hemostasis such as those with difficult bleeding, should be converted from selective to essential coverage. Going forward, when using catheters of 2mm (6Fr) or larger during vascular interventional procedures or after ECMO (extracorporeal membrane oxygenation) application and catheter removal where hemostasis is difficult, invasive hemostatic devices can be used and converted to essential coverage.
A pilot project will also be promoted to enhance the emergency abdominal surgery capabilities of regional surgical hospitals and establish cooperative systems. Regional hospitals (excluding tertiary general hospitals) that have at least three surgical specialists, including two full-time surgeons, perform more than 50 abdominal surgeries (62 types) annually such as appendectomy and bowel obstruction surgery, and are capable of 24-hour emergency abdominal surgery will receive a 100% additional fee for surgery and related anesthesia fees, with a temporary additional 100% increase until emergency care ends.
The 'Nurse Shift Improvement Pilot Project,' which has been underway since April 2022, will be extended until December 2027 to support nurses' work-life balance and regular, predictable shift work. Currently, 84 institutions including 43 tertiary general hospitals and 38 general hospitals are participating in this project, which supports personnel costs for additional nurses to cover emergency vacancies and ward operations, as well as education nurses for new nurse adaptation. A Ministry of Health and Welfare official said, "Based on the results of the first pilot project operated until the end of April this year, we will supplement shortcomings and more closely evaluate the effectiveness of the project in the second phase, expecting it to improve nurses' work quality and contribute to creating a stable medical environment."
© The Asia Business Daily(www.asiae.co.kr). All rights reserved.